Skin grafting is one of the most common treatment options for permanent replacement of lost skin and proven effective in burn patients. The procedure consists of transplantation of skin or artificial dermal replacements, and in some instances underlying tissues, harvested from one anatomical location to a different location. However the ischemic insult, due to nature of the procedure itself, on the graft tissue is the major problem for the graft integration and durability. By adding the increase in the number of severe full-thickness skin injuries both in civilian and military settings to the burn injuries, the need for efficient, safe, and cost-effective supplemental therapeutics is obvious to avoid graft failures, revision surgeries and expenses associated with care for these patients. The success of the skin graft integration and viability of the graft is highly dependent on the revascularization, suppression of over-exuberant inflammation and control of the infections.
Extracorporeal shock wave therapy (ESWT) has been shown to have beneficial effects in soft tissue wounds through increase in perfusion, angiogenesis and suppression of inflammation.
The objective of this study was to evaluate effects of single and repeated ESWT on skin graft survival and healing.
A total of 30 female Wistar rats (300–400 gr) were used in this study. All animals underwent surgical procedure of creating abdominal fullthickness skin grafts. 10 animals were assigned into Controls, ESWT-1 (one treatment, day 0), and ESWT-2 (repeated, days 0 and 4 after surgery). Animals received a total of 300 impulses across the entire region of the graft with an energy flux densitiy 0.1 mJ / mm2 (dermagold100, OP155, MTS Medical UG). Full-thickness biopsies were collected on days 4, 6, 9 and 12 after the surgery. Morphological and histological evaluation of skin grafts was performed. Time-to-heal, skin graft thickness, number of capillaries, and degree of inflammation was assessed.
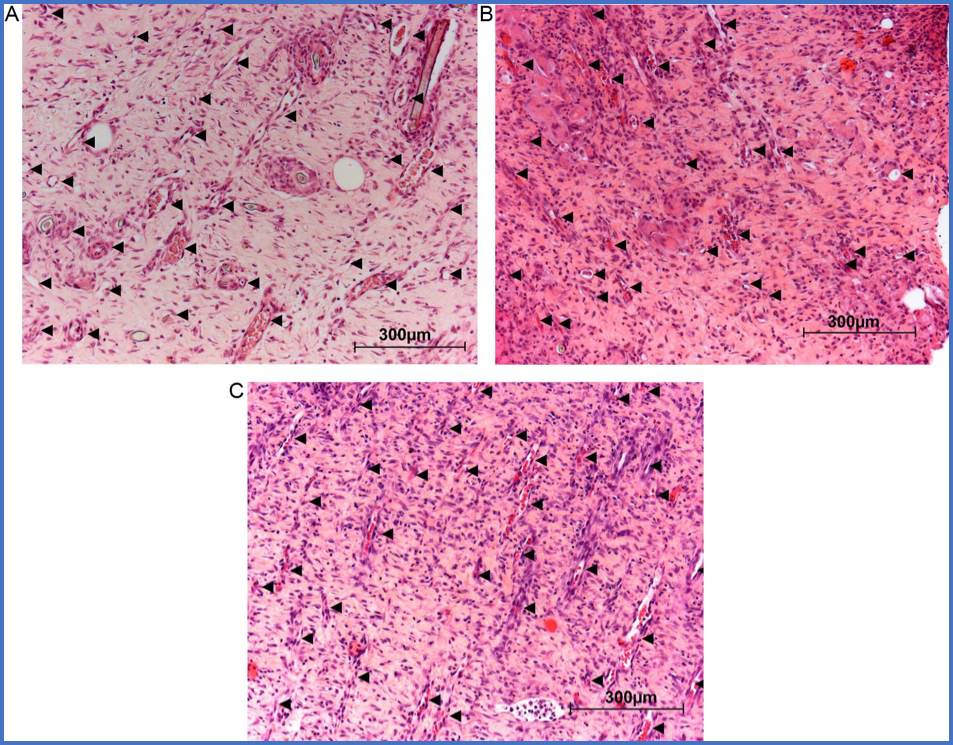
Macroscopic evaluation showed similar healing rate in all groups. They observed an increase in thickness of skin grafts starting at day 6 in ESWT treated groups. There was an increase in capillary density in ESWT-1 on day 12 and ESWT-2 at day 9 and 12. Increase in immune cell infiltration in both ESWT treated groups in comparison to Controls was observed.
Figure 3. Number of capillaries in the three bright fields per skin layer were counted and represented as mean+/−SEM. ESWT induced increase in the number of capillaries in both groups (B- ESWT-1; C- ESWT-2) in comparison to Control (A) on Day 12. Importantly, repeated ESWT induced these effects at earlier time points (Day 9) and to higher extent (Day 12) when compared to ESWT-1. * p < 0.05 vs Control; +p < 0.05 vs ESWT-1.
Beneficial effects of Spark Wave Therapy:
- Induces skin graft thickening
- Beneficial structural effect on skin grafts
- Increases number of capillaries
- Increases tissue perfusion:
- By rapid release of nitric oxygen
- By sustainable formation of new blood and lymph vessels
- Triggers cellular responses favorable for healing and regeneration
- Improves wound healing
- Non-invasive
- Easy to apply
- No side effects, minimal risks
- Cost-effective
- Efficient supplemental treatment for challenging wound healing processes
Extracorporoeal shock wave therapy is a non-invasive, promising new modality for the use in soft tissue indications. This study has demonstrated that Spark Wave Therapy has beneficial structural effects on the skin grafts and increases the number and the denisty of blood vessels within the graft tissues, but warrants further investigations about the timing and number of treatments.
Reference: