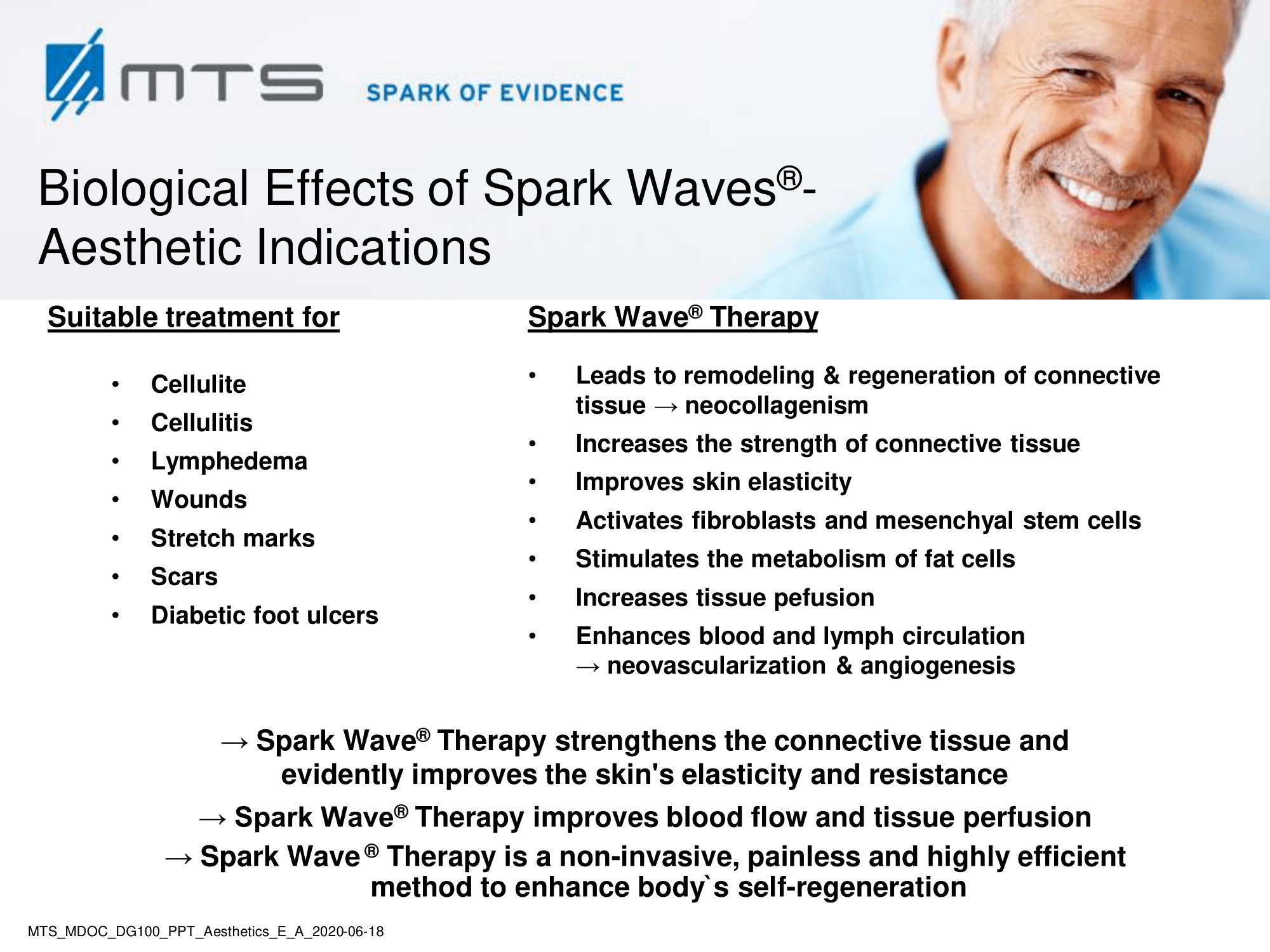
MTS Spark Waves®– an effective therapy option for aesthetic indications
Cellulite / Scars / Stretch marks / Lymphoedema / Alopecia
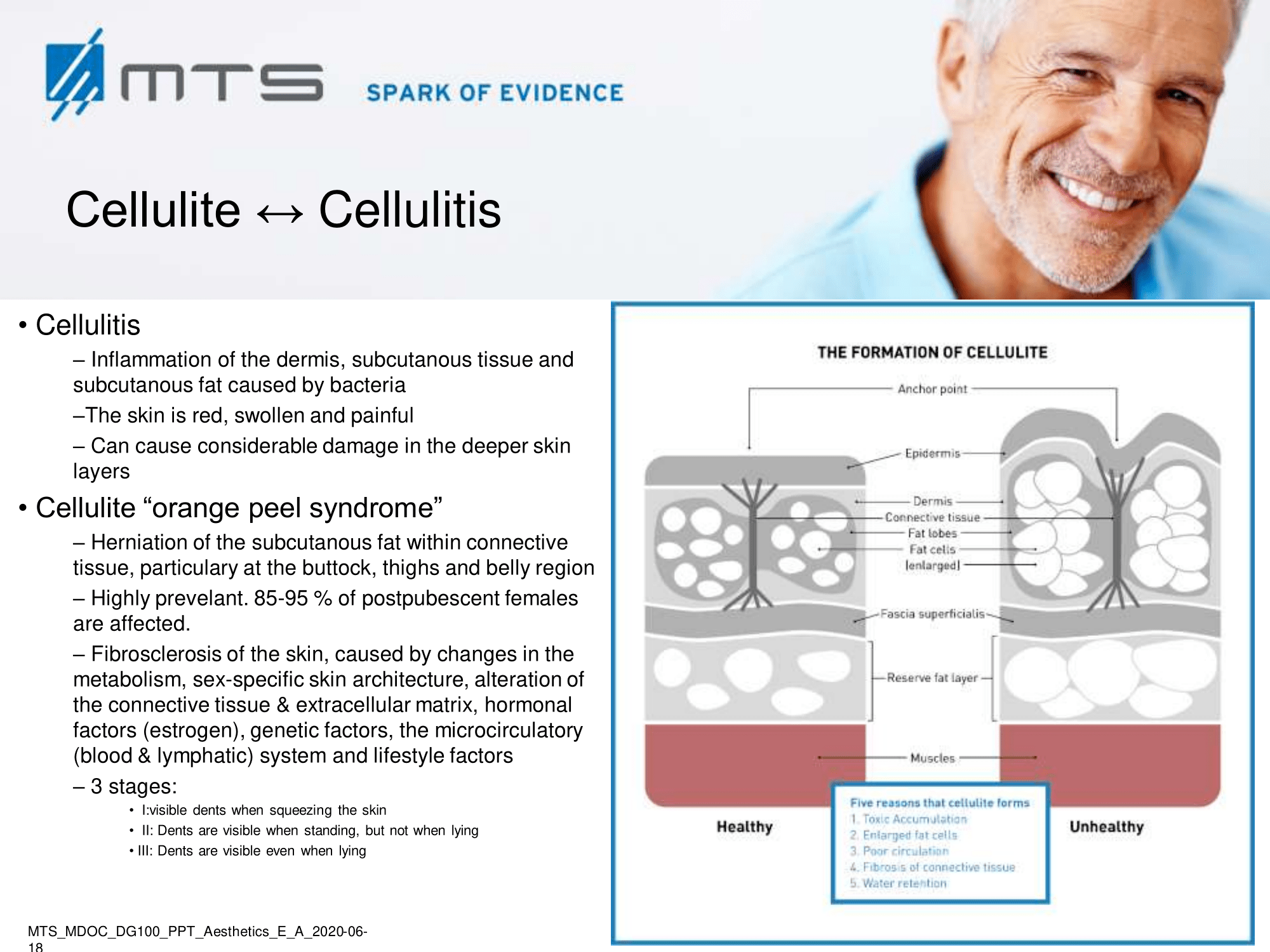
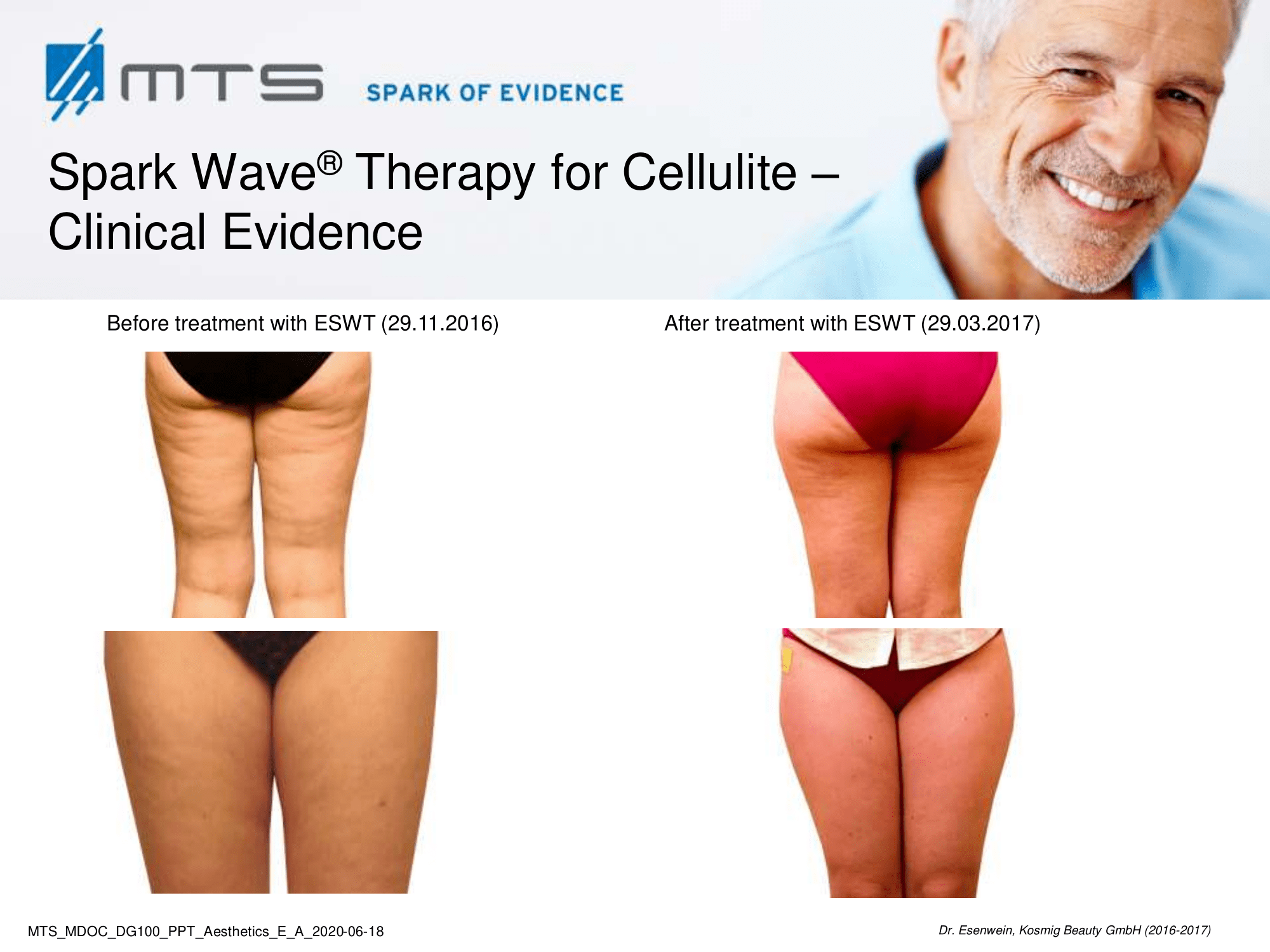
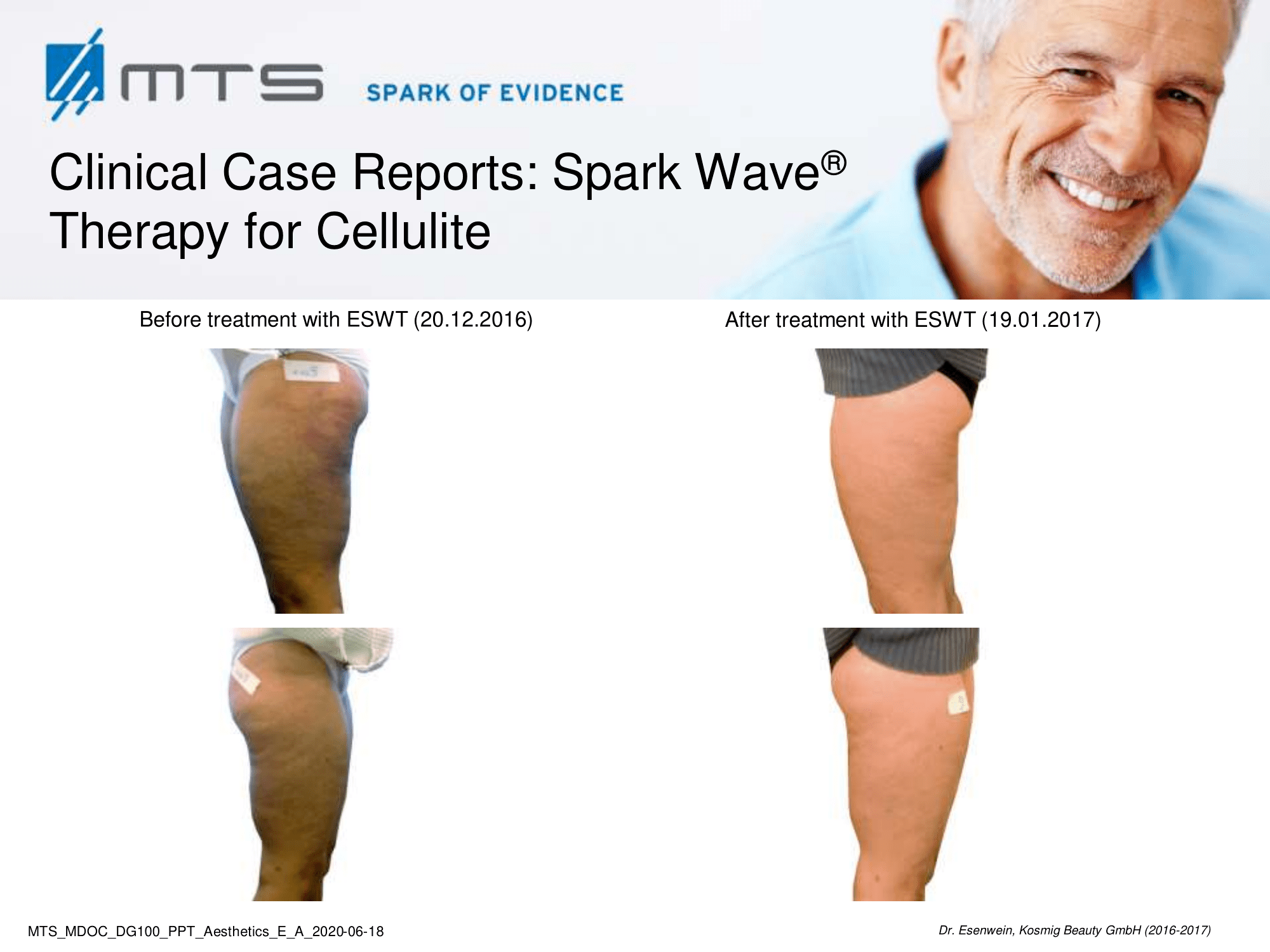
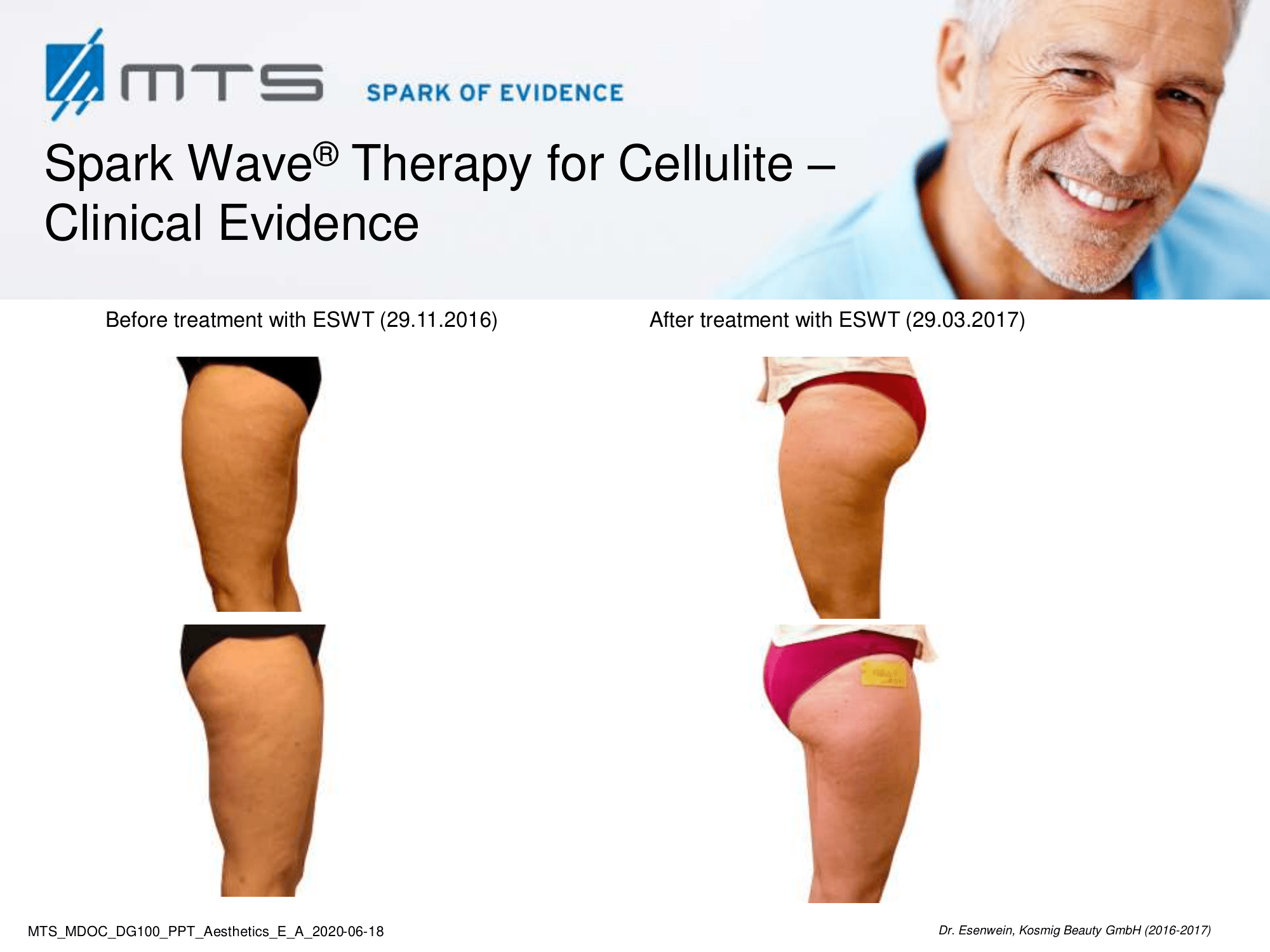
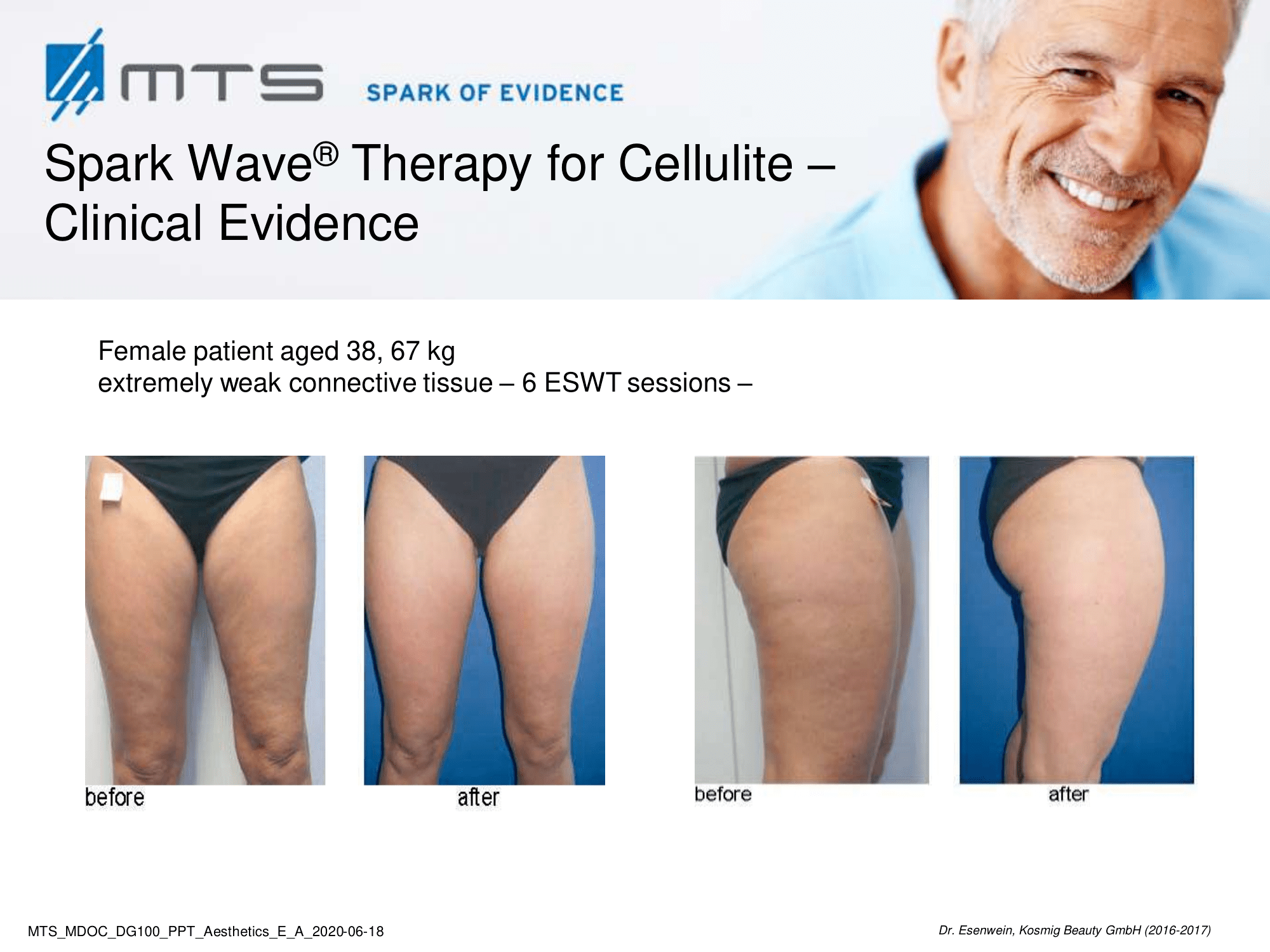
Cellulite is a multifactorial condition that is present in 80-90 % of post-pubertal women, commonly found on the posterolateral thighs, buttocks, and abdomen. It is described by an orange peel appearance of the skin surface and classified into four grades. Despite its high prevalence, it remains a major concern for women. Cellulite is a multifactor condition that requires a multidisciplinary approach for the treatment. Factors include, among others, connective tissue architecture, estrogen action, microvascular alterations, and certain genetic and hormonal characteristics. Inadequate nutrition and poor lifestyle tend to worsen the appearance of cellulite. Body fat, stress, fatty, sugary and salty food, inactivity, alcohol and smoking favour cellulite.
Benefits of Spark Wave® Therapy for cellulite:
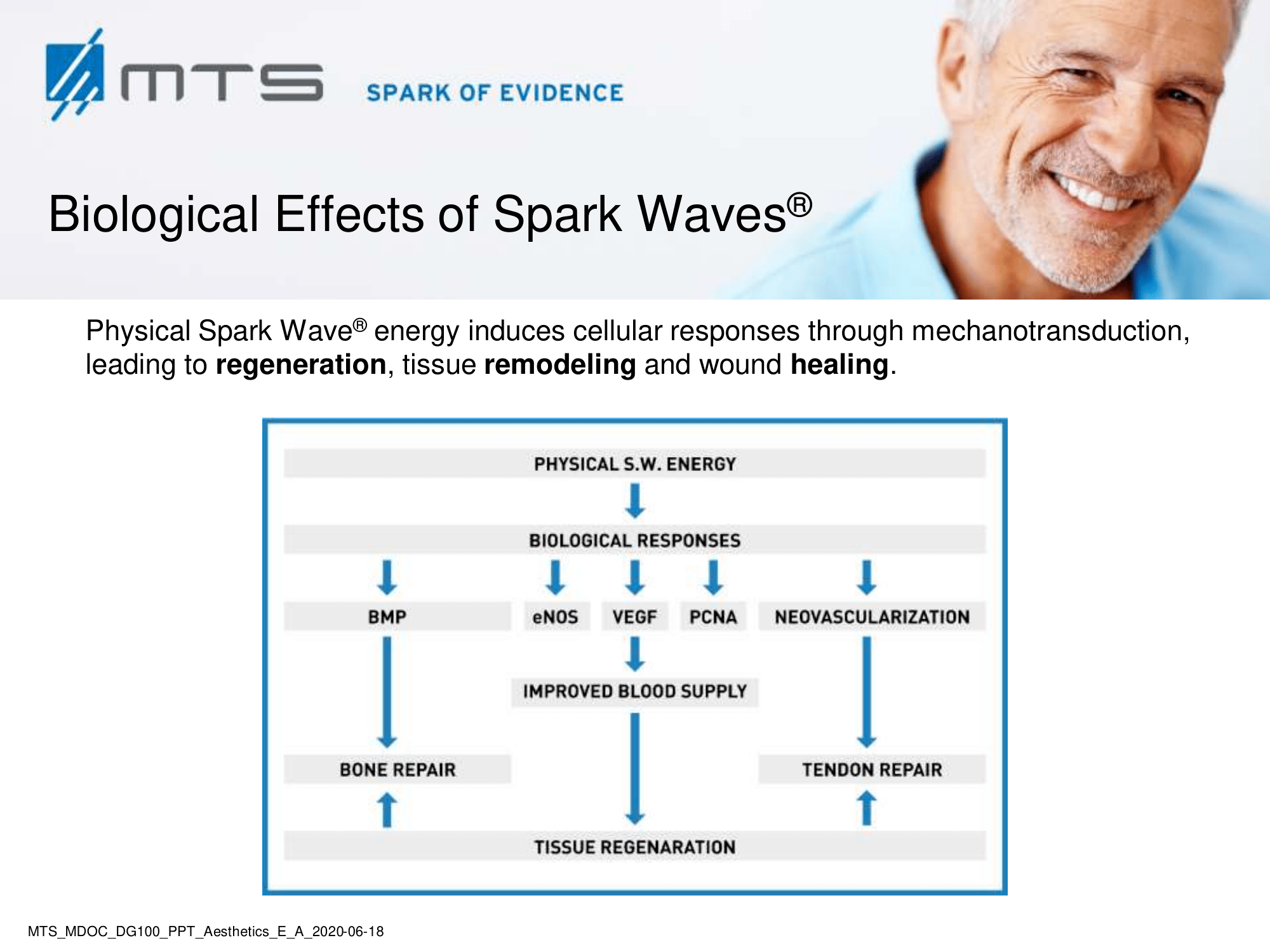
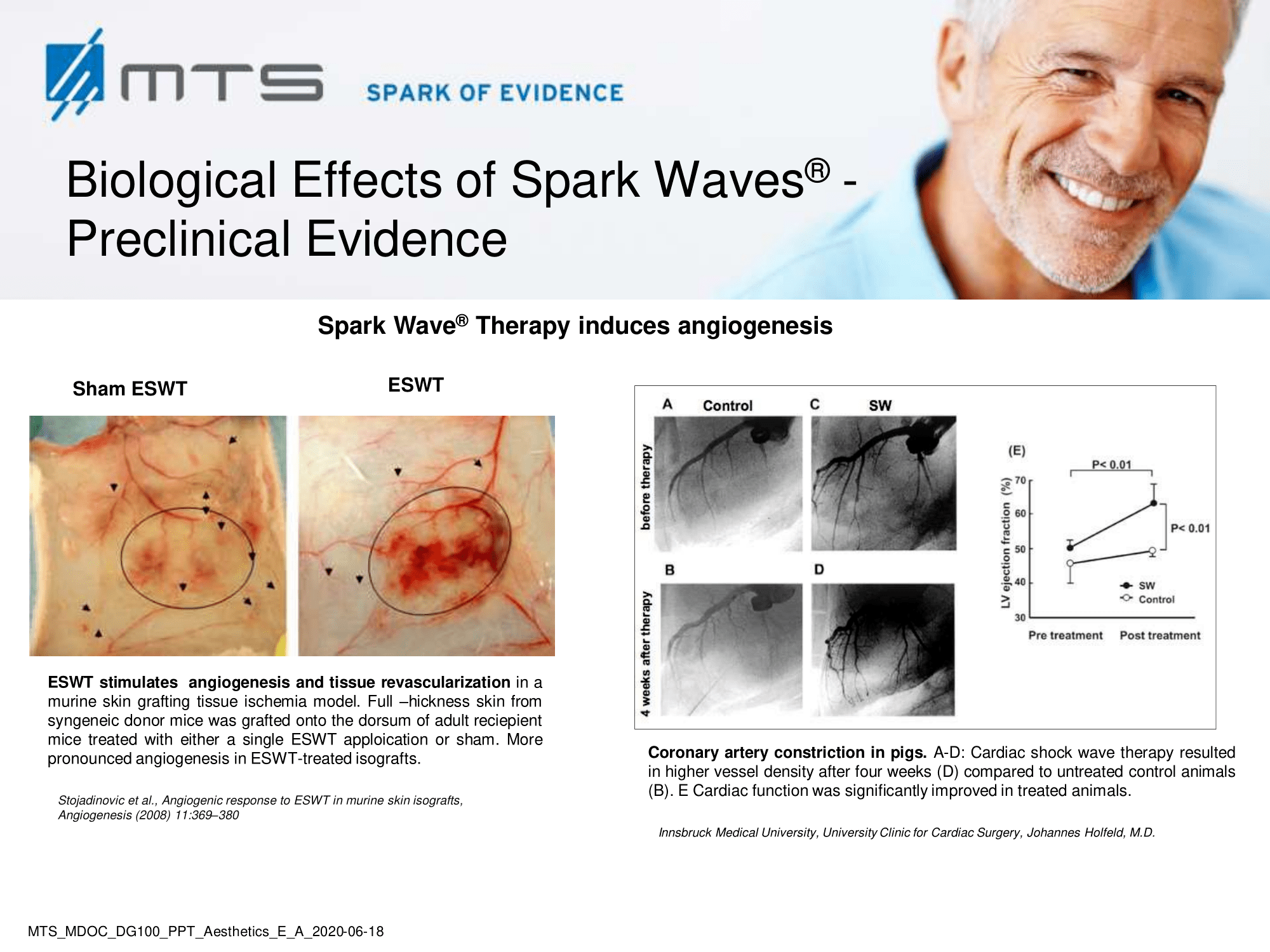
Extracorporeal shock wave therapy (ESWT) improves local blood circulation via neovascularization and increases cell proliferation of collagen and elastin fibers, which subsequently improves skin elasticity and revitalization of the dermis. ESWT has a positive effect on lymphoedema / lipedema by promoting lymph transport (lymphatic drainage), which is a pathway often associated with cellulite. In vitro tests have further shown that it may increase cell permeability, which may stimulate the exchange of fat cells and activate phospholipases through the beta-receptors on the fat cells’ membrane. 1
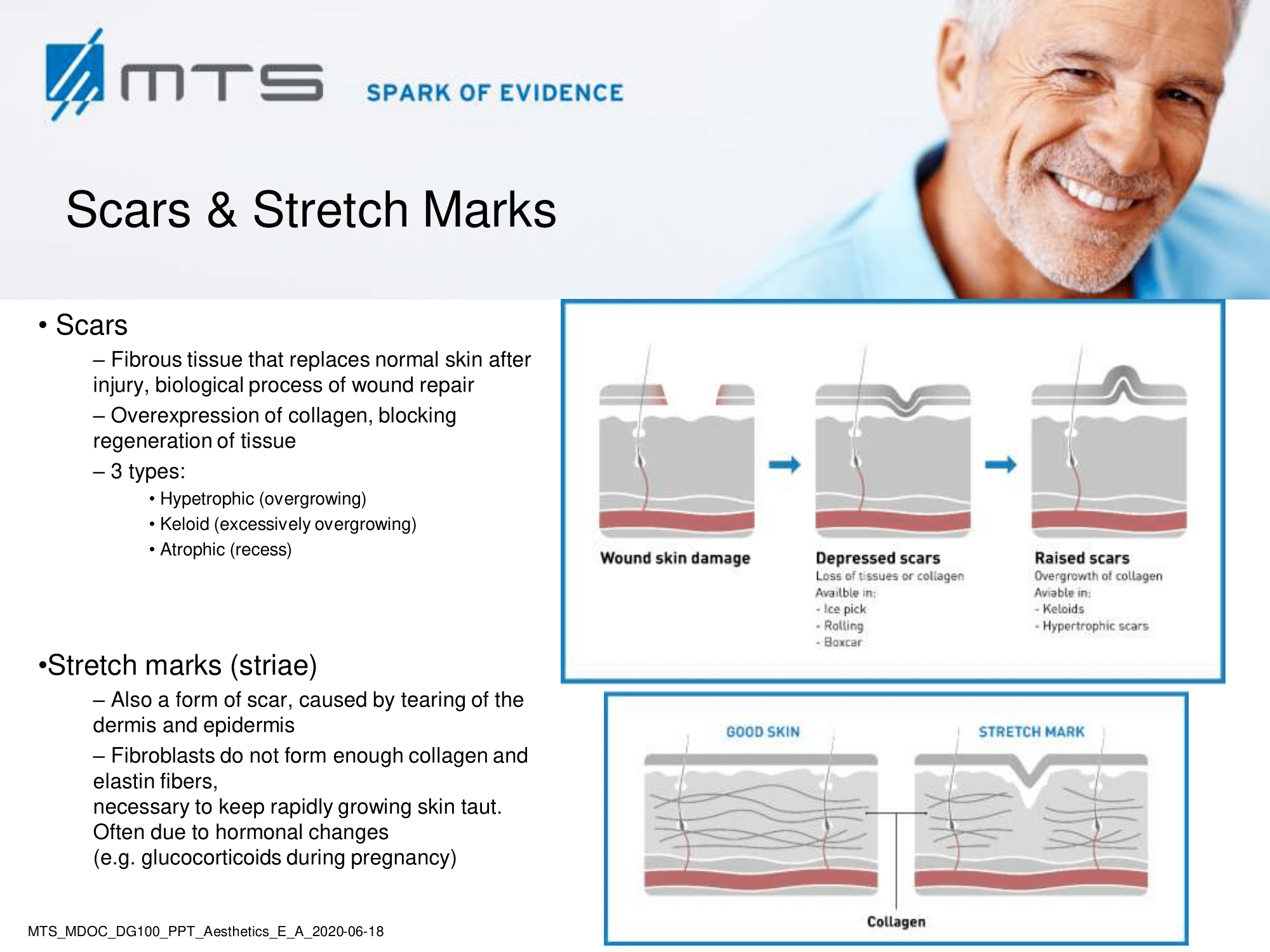
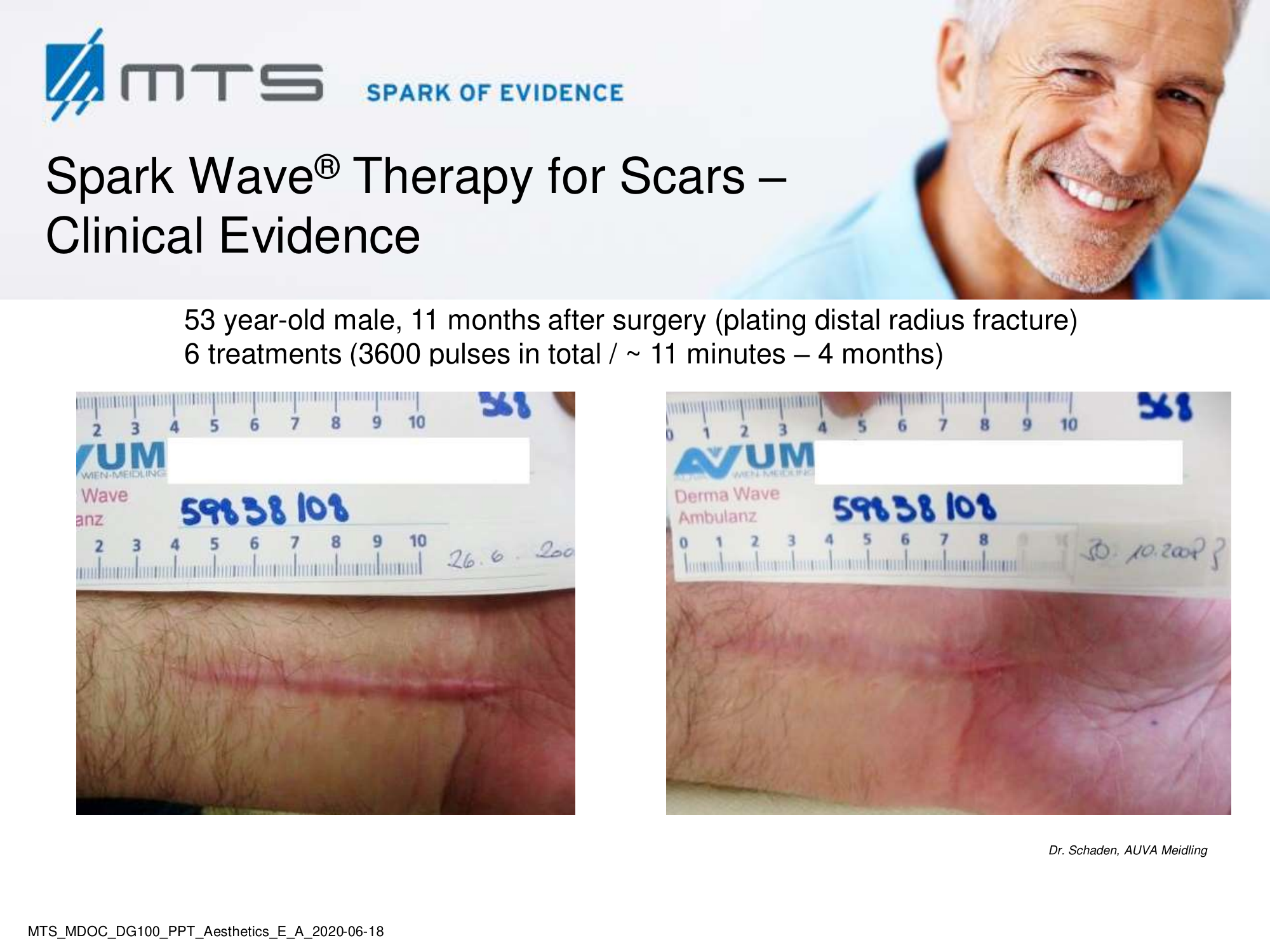
A scar is fibrous tissue that leaves after wound healing due to injury, sores or burns. Abnormal scarring remains a burdensome functional and aesthetic consequence for affected patients. The International Advisory Panel on Scar Management developed a grading system to distinguish different classes of scars. 2 A variety of measurement tools are applied such as pigmentation, vascularity, thickness, pliability, height or depression, patient acceptability and comfort. Immature scars are in the process of remodeling. They appear red and mildly elevated with patients reporting pain and pruritus. Most immature scars mature normally and become lightly colored and flat. However, they may also develop into pathologic scars, classified into atrophic and hypertrophic scars, with the latter being further subdivided into simple hypertrophic and keloid scars. 2 Retracting scars are characterized by collagen fibers in a cord-like disposition exerting significant traction on surrounding healthy tissue and may cause significant functional deficit and pain. 3 Local and systemic factors appear to be able to contribute and to promote pathologic scarring: wound features, extent of bleeding, presence of hematoma and serum collection, superimposing infection, innervation deficits, constitutional characteristics of the patient, co-administration of drugs, blood supply disorders, lack of nutritional factors and endocrine disorders.4
Benefits of Spark Wave® Therapy for scars:
ESWT was shown to effectively promote wound healing in acute and chronic soft tissue wounds, burn lesions and diabetic foot ulcers. Treated lesions showed increased cell activity and proliferation, decreased apoptosis and tissue necrosis and an improvement in blood flow and tissue regeneration. 5
ESWT mechanically stimulates receptors of the extracellular matrix and activates fibroblasts to convert into myofibroblasts which finally mediate wound repair. The precise mechanism underlying abnormal scarring is not yet clearly understood and there are several hypotheses. However, the right cell population equilibrium (fibroblasts, myofibroblasts, keratinocytes) and a properly balanced expression of all factors involved (growth factors and cytokines, e. g. TGF-ß, PDGF, fibronectin, hyaluronic acid, biglycan, collagen…) are essential for normal skin healing. Pathophysiological scar formation includes dysregulation of microcellular actors and processes which in turn leads to abnormal collagen synthesis. 6 Research results and clinical evidence indicate, that ESWT rebalances activation, proliferation, synthesis and differentiation of the connective tissue.
According to current basic research in hypertrophic scar-derived primary human fibroblasts in vitro suggested that unchanged viability, reduced migration and the suppressed expression of typical epithelial-mesenchymal transition markers might be involved in the ESWT anti-scar effect. 7 In an animal model of hypertrophic scar in a rabbit ear, ESWT was able to suppress scar formation and to improve some characteristics of the scar texture. 6,8 In clinical studies ESWT improved scar pain and pruritus, and the overall appearance of atrophic and hypertrophic (burn) scars. 3,9–11 A very recent comparative study by Wang et al. demonstrated that ESWT is comparably effective in the treatment of keloid scars as local steroid injections. 12
ESWT is an effective non-invasive therapy option in the management of scars. It seems to have a significant benefit in the support of a fresh scar and the prevention of pathologic scar formation since it accelerates reepithelialization, acts anti-inflammatory, enhances tissue perfusion and blood flow thereby leading to improved skin regeneration and tissue remodeling. 13,14
Stretch marks (striae distensae) are narrow scars at the skin that occur when there is a sudden stretch of the skin due to obesity, puberty, pregnancy, steroid medication and a quick weight gain. Familiar genetic predisposition may also play a role. They form at the thighs, abdomen, breasts, hips, lower back and upper arms when the dermis is overstretched and tears. Stretch marks do not cause health problems but can evoke psychological discomfort and affect quality of life. Sometimes stretch marks cause burning and itching and in rare cases, healing disorders can lead to swelling and inflammation of the affected skin. Dependent on their etiology, striae are divided into striae atrophica, striae distensae (rubrae, albae) and striae gravidanum. Depending on the race and age of the population studied, the prevalence of stretch marks has been reported to range from 50 % to 90 %. A reduction in risks can be achieved by using a rich skin care, a balanced diet, exercise, avoidance of big and rapid weight variations and maintenance of a healthy weight.
Benefits of Spark Wave® Therapy for stretch marks:
ESWT is thought to improve the appearance and to reduce the symptoms associated with stretch marks by promoting the following processes; increased collagen production and fibroblastic activity, increase in elasticity and blood perfusion, improvement in cell proliferation, increased skin hydration and anti-inflammatory properties. 15
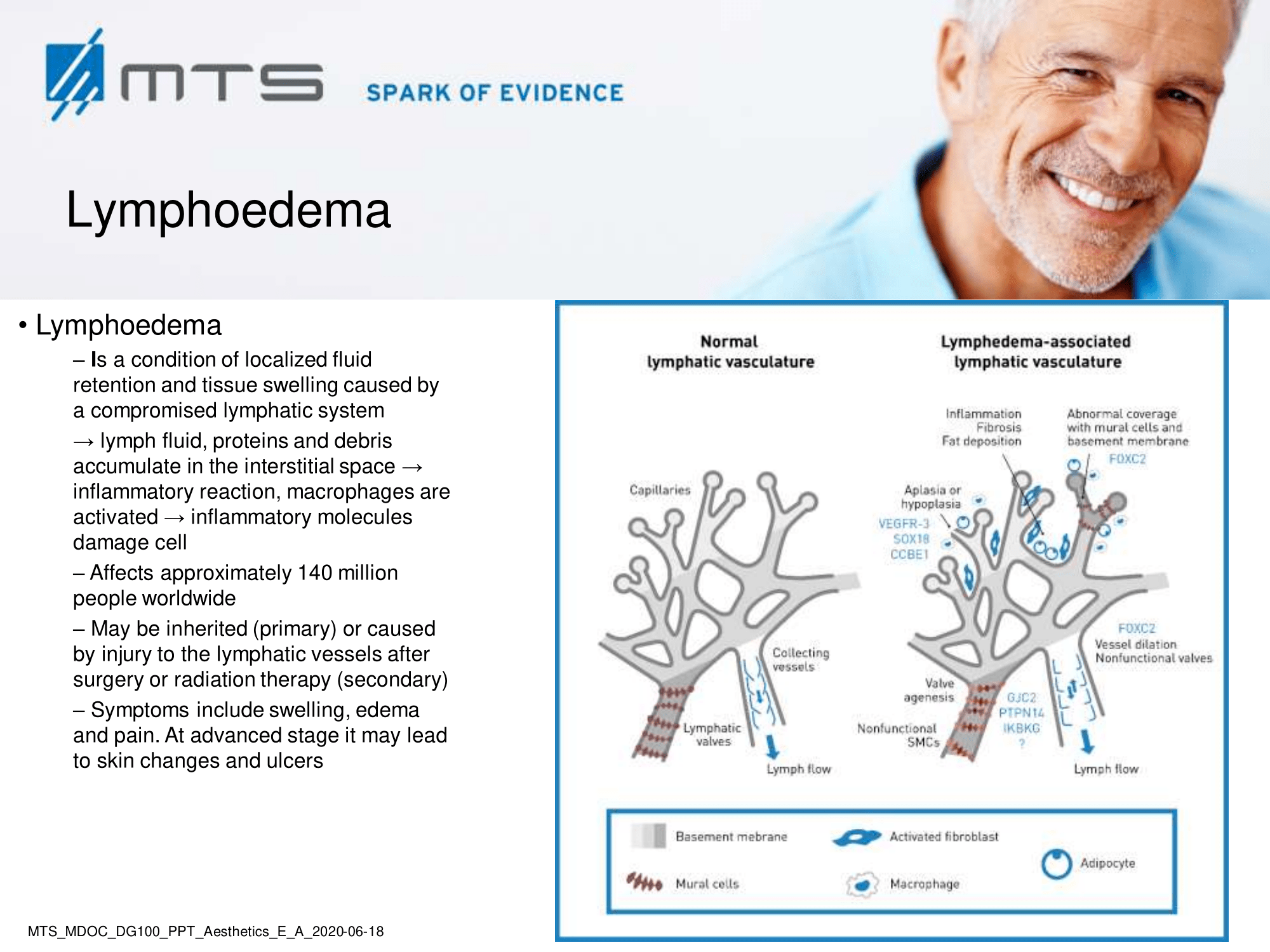
Lymphoedema is a common progressive and often debilitating disease caused by the accumulation of protein-rich fluid in the interstitial spaces due to insufficiency of the lymphatic system. 16 Lymph stasis induces an inflammatory reaction that leads to the proliferation of adipose tissue and to fibrosis, resulting in mild to severe and permanent swelling of the affected body parts. 17 Its nature can be acute, transitory or chronic. It is divided into primary (congenital) or secondary (acquired) lymphoedema. The primary form is due to abnormal lymphangiogenesis in utero and often connected to associated genes. Secondary lymphoedema can be the consequence of malignancies, trauma, surgery, infection, anti-inflammation or radiation therapy. Systemic causes of lymphoedema could be congestive heart failure, liver cirrhosis, glomerulonephritis, hyper- or hypothyroidism, enteropathies or iatrogenic (e . g. medications). Secondary lymphoedema is more common than primary and in the western world cancer surgery and radiation therapy are its most common causes. Severity of lymphoedema is basically classified into four clinical stages (defined by the International Society of Lymphology, ILS).
Benefits of Spark Wave® Therapy for lymphoedema:
The underlying mechanism of action of ESWT in lymphoedema was shown in vitro and in animal models, where it increased cell permeability, promoted lymphangiogenesis and enhanced lymphatic endothelial cell proliferation. ESWT stimulates lymphatic drainage and microcirculation. According to a recent review, shock wave therapy in the treatment of lymphoedema enhances cellular metabolism and has an anti-inflammatory, vasodilatory and neo-angiogenic effect. 17
Alopecia. Male pattern hair loss (MPHL) and female pattern hair loss (FMPH) are typically experienced as a “moderately stressful condition that diminishes body image satisfaction”. Deleterious effects on self-esteem and certain facets of psychological adjustment are more apparent among women than men and among treatment-seeking patients 18. Pattern hair loss by the age of 50 affects about half of males and a quarter of females and represents the most common cause of baldness. 19
Conventional therapy includes medical treatment like Minoxidil, an antihypertensive vasodilator. Hypothetically, it is thought to widen blood vessels allowing increased flow of oxygen, blood and nutrients to the follicles. Its success is moderate and the treatment is not suitable for every patient. Another possibility of intervention is Finasteride, a 5α-reductase inhibitor, interfering with the hormonal balance of the body and bearing the potential of unintended side-effects like e.g. erectile dysfunction or depression (post-finasteride syndrome). Finally, invasive and painful procedures as hair transplant surgery are performed.
Recent reports of the international society of shock wave therapy (ISMST) observed hair growth-promoting side effects on the skin of shock wave-exposed areas during the treatment of other indications and suggested it as a potential therapy for baldness. It is also already used by some aesthetic centers.
Benefits of Spark Wave® Therapy for alopecia
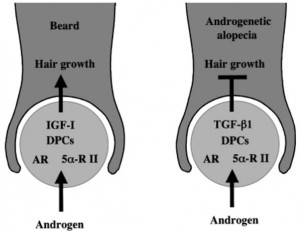
PHL is thought to be due to a combination of genetic and hormonal factors. In hair follicles, 5α-reductase type 1 and 2, androgen receptors (AR) and AR coactivators can regulate androgen sensitivity of dermal papillae (DP). To regulate hair growth, androgens regulate production of growth factors and cytokines like IGF-1 (insulin growth factor), TGF-β1 (transforming growth factor), TGF-β2, and ILs (interleukins). In addition, androgens enhance inducible NOS (nitric oxide synthase) from occipital DP cells and stem cell factors for regulation of hair growth. Moreover, androgenic alopecia involves crosstalk between androgen and Wnt/β-catenin signalling. 20
Schematic diagram of androgen action of human hair follicles. For the beard growth stimulation by androgen, insulin-like growth factor-I (IGF-I) acts as the paracrine mediator from dermal papilla cells (DPC) to epithelial cells. On the other hand, transforming growth factor-b1 (TGFb1) is an androgen-dependent paracrine mediator for androgenetic alopecia. 21
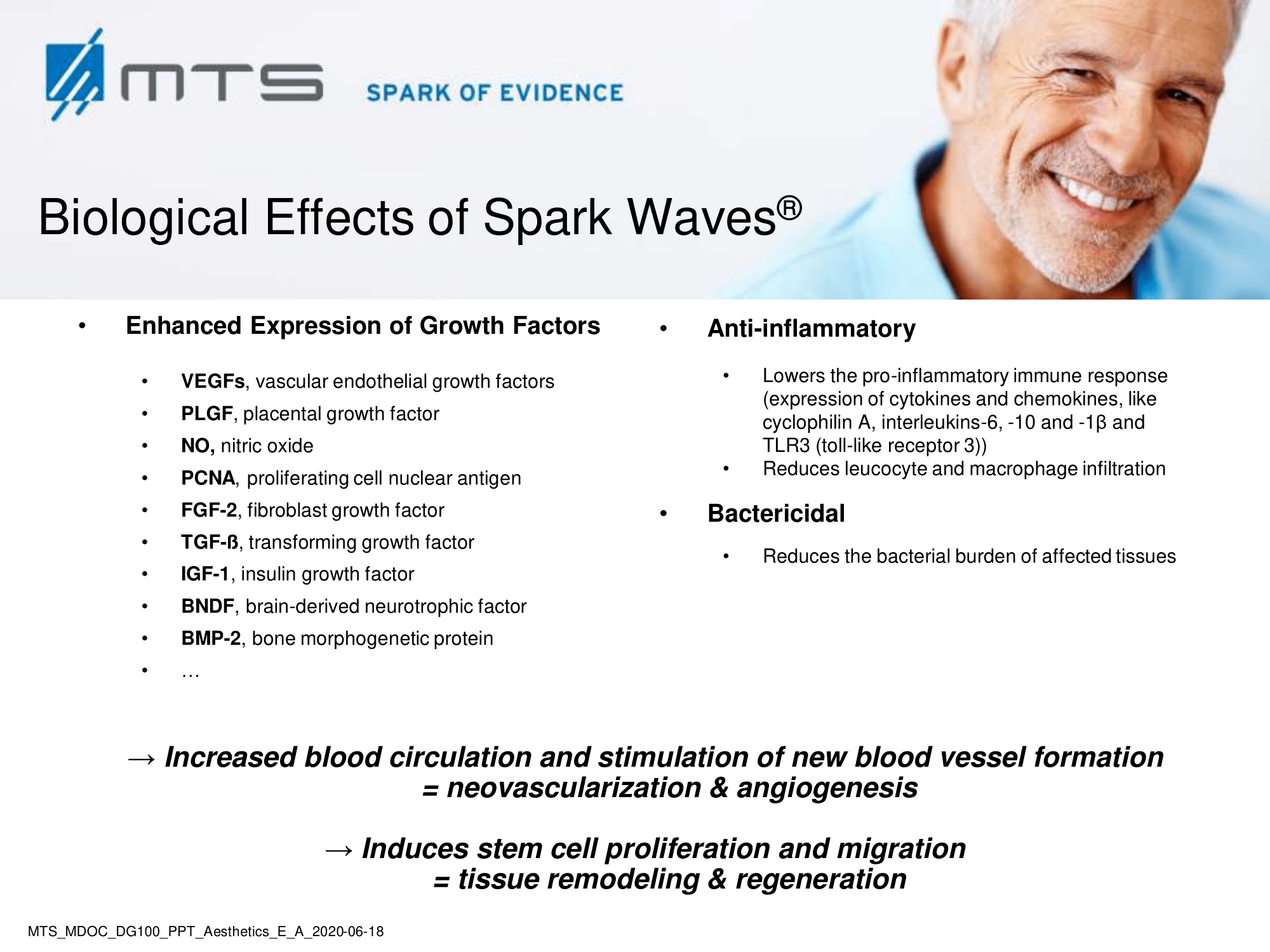
It was previously shown, that ESWT induced activation of numerous growth factors like endothelial NOS (nitric oxide synthase), IGF (insulin-like growth factor), TGF-ß (transforming growth factor), VEGF (vascular endothelial growth factor), FGF (fibroblast growth factor), ILs (interleukins) and PCNA (proliferating cell nuclear antigen) leading to angiogenesis and revascularization in the affected areas. 22–24 NO evels are elevated upon SWT which enhances tissue perfusion, partially due to the increased performance of nitric oxide synthase (NOS). 25–27 NO , as a potent vasodilator, leads to improved blood and nutrient supply of the tissue and increases overall blood circulation. Hence, by mechanotrunsduction, SWT strongly induces cascades of cell proliferation, tissue remodelling and regeneration. 28
Microneedling is a relatively new, minimally invasive procedure involving superficial and controlled puncturing of the skin by rolling with fine miniature needles. It was initially introduced for skin rejuvenation, however, now it is used for a wide range of indications including acne scars, post-traumatic / burn scars, alopecia, skin rejuvenation, drug delivery, hyperhidrosis, stretch marks and many more.29 Micropunctures are created using microneedles which produce a controlled skin injury without actually damaging the epidermis. These microinjuries lead to minimal superficial bleeding and set up a wound healing cascade with release of various growth factors such as platelet derived growth factor (PGF), transforming growth factor alpha and beta (TGF-α and TGF-β), connective tissue activating proteins, connective tissue growth factors, and fibroblast growth factor (FGF).29 The use of microneedling over scalp for alopecia is one of its recent advances but already some preliminary, encouraging studies have been performed. 30–33
Our new concept of Spark Wave-assisted, minimally invasive treatment of adrogenic alopecia combined with microneedling represents a cost-effective, therapeutic alternative to surgical hair transplant.
Under research:
The concept of Spark Wave® Therapy-assisted treatment of androgenic alopecia:
a therapeutic alternative to surgical hair transplant?
The concept
The dermaroller with microneedles of medical grade, usually 0.5 – 3 mm long, will create microdamages to the epidermis and dermis by rolling action. This results in activation of body’s own repair mechanism. When applied to the scalp, it will increase the number of hair follicles and also strengthen and accelerate growth of the existing hair. However, due to a certain restriction of body’s own repair mechanism (homeostasis), the therapeutic effects are still limited. When assisted by SWT, which on its own leads to fast and intensive hair growth, drastic changes can be expected. On the basis of induced angiogenesis and regeneration the microneedling and SWT will lead to rapid hair growth as sufficient blood supply is crucial for maintenance, repair and growth of new hair follicles.
The perspectives
The combination therapy using microneedling and SWT-assisted treatment of andogenic alopecia will exponentiate the outcome of enhanced hair growth. It is an office-based procedure consisting of multiple sittings which are minimally invasive and very cost-effective. The risk of unintended side-effects is very low and adverse events are really uncommon. 34 The concept can be considered a safe and gentle alternative to surgical hair transplant. Due to its novelty, clinical trials are required to evaluate its efficacy.
The concept was invented together with Mirza Niaz Zaman, MD (General Medicine, 5th course), KNMU, Ukraine. If you are interested to discuss this project or want to manage or participate in a clinical trial please feel free to directly contact us for further discussion.
References
- Luebberding, S., Krueger, N. & Sadick, N. S. Cellulite: An Evidence-Based Review. American Journal of Clinical Dermatology (2015). doi:10.1007/s40257-015-0129-5
- Mustoe, T. A. et al. International clinical recommendations on scar management. Plast. Reconstr. Surg. (2002). doi:10.1097/00006534-200208000-00031
- Saggini, R. et al. Etracorporeal shock wave therapy: An emerging treatment modality for retracting scars of the hands. Ultrasound Med. Biol. 42, 185–195 (2015).
- Widgerow, A. D. Cellular/extracellular matrix cross-talk in scar evolution and control. Wound Repair and Regeneration (2011). doi:10.1111/j.1524-475X.2010.00662.x
- Zhang, L. et al. Efficacy and safety of extracorporeal shock wave therapy for acute and chronic soft tissue wounds: A systematic review and meta-analysis. International Wound Journal (2018). doi:10.1111/iwj.12902
- Zhao, J. C. et al. Lower energy radial shock wave therapy improves characteristics of hypertrophic scar in a rabbit ear model. Exp. Ther. Med. (2018). doi:10.3892/etm.2017.5441
- Cui, H. S. et al. Extracorporeal shock wave therapy alters the expression of fibrosis-related molecules in fibroblast derived from human hypertrophic scar. Int. J. Mol. Sci. (2018). doi:10.3390/ijms19010124
- Zhao, J. C. et al. Extracorporeal shock wave therapy with low-energy flux density inhibits hypertrophic scar formation in an animal model. Int. J. Mol. Med. (2018). doi:10.3892/ijmm.2018.3434
- Taheri P, Khosrawi S, Mazaheri M, Parsa MA, M. A. Effect of extracorporeal shock wave therapy on improving burn scar in patients with burnt extremities in Isfahan, Iran. J Res Med Sci. 23, (2018).
- Cho, Y. S. et al. Effect of extracorporeal shock wave therapy on scar pain in burn patients: A prospective, randomized, single-blind, placebo-controlled study. Medicine (Baltimore). 95, e4575 (2016).
- Fioramonti, P. et al. Extracorporeal shock wave therapy for the management of burn scars. Dermatologic Surg. (2012). doi:10.1111/j.1524-4725.2012.02355.x
- Wang, C. J., Ko, J. Y., Chou, W. Y., Cheng, J. H. & Kuo, Y. R. Extracorporeal shockwave therapy for treatment of keloid scars. Wound Repair Regen. (2018). doi:10.1111/wrr.12610
- Ottomann, C. et al. Prospective Randomized Phase II Trial of Accelerated Reepithelialization of Superficial Second-Degree Burn Wounds Using Extracorporeal Shock Wave Therapy. Ann. Surg. 255, 23–29 (2012).
- Arnó, A. et al. Extracorporeal shock waves, a new non-surgical method to treat severe burns. Burns 36, 844–849 (2010).
- Ud-Din, S., McGeorge, D. & Bayat, A. Topical management of striae distensae (stretch marks): Prevention and therapy of striae rubrae and albae. Journal of the European Academy of Dermatology and Venereology (2016). doi:10.1111/jdv.13223
- The diagnosis and treatment of peripheral lymphedema: 2016 consensus document of the International Society of Lymphology. Acta Angiol. (2017). doi:DOI 10.1016/j.tsf.2007.03.176
- Yüksel A, Gürbüz O, Velioğlu Y, Kumtepe G, Ş. S. Management of lymphoedema. Vasa. 45, 283–91 (2016).
- T.F., C. The psychosocial consequences of androgenetic alopecia: A review of the research literature. Br. J. Dermatol. 141, 398–405 (1999).
- Vary, J. C. Selected Disorders of Skin Appendages-Acne, Alopecia, Hyperhidrosis. Medical Clinics of North America 99, 1195–1211 (2015).
- Inui, S. & Itami, S. Androgen actions on the human hair follicle: Perspectives. Exp. Dermatol. 22, 168–171 (2013).
- Itami, S. & Inui, S. Role of Androgen in Mesenchymal Epithelial Interactions in Human Hair Follicle. J. Investig. Dermatology Symp. Proc. 10, 209–211 (2005).
- Pfaff, J. A., Boelck, B., Bloch, W. & Nentwig, G.-H. Growth Factors in Bone Marrow Blood of the Mandible With Application of Extracorporeal Shock Wave Therapy. Implant Dent. 25, 606–612 (2016).
- Cai, H. Y. et al. Cardiac shockwave therapy improves myocardial function in patients with refractory coronary artery disease by promoting VEGF and IL-8 secretion to mediate the proliferation of endothelial progenitor cells. Exp. Ther. Med. 10, 2410–2416 (2015).
- Xin, Z., Liu, J., Wang, L. & Li, H. [Progress of low-energy shockwave therapy in clinical application]. Beijing Da Xue Xue Bao. 45, 657–60 (2013).
- Mittermayr, R. et al. Extracorporeal shock wave therapy (ESWT) for wound healing: Technology, mechanisms, and clinical efficacy. Wound Repair and Regeneration 20, 456–465 (2012).
- Gotte, G. et al. Short-time non-enzymatic nitric oxide synthesis from L-arginine and hydrogen peroxide induced by shock waves treatment. FEBS Lett. 520, 153–155 (2002).
- Antonic, V., Mittermayr, R., Schaden, W. & Stojadinovic, A. Evidence Supporting Extracorporeal Shockwave Therapy for Acute and Chronic Soft Tissue Wounds. WOUNDS-A Compend. Clin. Res. Pract. 23, 204–215 (2011).
- Wang, C.-J., Wu, R.-W. & Yang, Y.-J. Treatment of diabetic foot ulcers: A comparative study of extracorporeal shockwave therapy and hyperbaric oxygen therapy. Diabetes Res. Clin. Pract. 92, 187–193 (2011).
- Singh, A. & Yadav, S. Microneedling: Advances and widening horizons. Indian Dermatol. Online J. 7, 244–254 (2016).
- Dhurat, R. et al. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: a pilot study. Int. J. Trichology 5, 6–11 (2013).
- Farid, C. I. & Abdelmaksoud, R. A. Platelet-rich plasma microneedling versus 5% topical minoxidil in the treatment of patterned hair loss. J. Egypt. Womenʼs Dermatologic Soc. 13, 29–36 (2016).
- Dhurat, R. & Mathapati, S. Response to Microneedling Treatment in Men with Androgenetic Alopecia Who Failed to Respond to Conventional Therapy. Indian J Dermatol. 60, 260–3
- Chandrashekar, B., Yepuri, V., Mysore, V. & Charmalaya, V. Alopecia Areata—Successful Outcome with Microneedling and Triamcinolone Acetonide. J Cutan Aesthet Surg 7, 63–64 (2014).
- Hou, A., Cohen, B., Haimovic, A. & Elbuluk, N. Microneedling: A Comprehensive Review. Dermatol. Surg. 43, 321–339 (2017).