Ischemic heart disease remains the leading cause of mortality (12.7 %) worldwide, causing more than 7 million deaths per year.
Native angiogenesis after infarction most often is not sufficient for appropriate supply of hibernating cardiomyocytes, leading to pathologic left ventricle (LV) remodeling and ischemic cardiomyopathy, a clinical entity characterized by a poor prognosis and severe symptoms in affected patients. Management of this disease often is limited, and curative strategies beside heart transplantation are lacking. Therefore, therapies enhancing vascularization in the infarction zone by induction of capillary sprouting from existing vessels (angiogenesis) and/or by recruitment of bone marrow–derived endothelial cells (BMEC) for de novo vessel formation (vasculogenesis) are of high relevance.
At low energy levels, shock wave therapy (SWT) is in routine clinical use for the treatment of wound-healing disturbances, tendinopathies, and nonhealing bone fractures. The regenerative effects of SWT have been mainly attributed to the induction of angiogenesis via growth factor release. In preclinical experiments, shock wave-treated hearts showed an increased number of capillaries and arterioles in the infarction border zone, thereby leading to a significantly improved left ventricular ejection fraction. In clinical studies, SWT caused the improvement of angina symptoms in patients with ischemic heart disease.
Scientists of the group of Johannes Holfeld, MD, from the (University Clinic of Cardiac Surgery in Innsbruck, Austria) investigated the question whether mechanical stimulation upon Spark Wave Therapy improves heart function by induction of angiogenesis.
SWT was applied in a mouse model of chronic myocardial ischemia. To study effects of SWT on postnatal vasculogenesis, wild-type mice received bone marrow transplantation from green fluorescence protein donor mice. Underlying mechanisms were elucidated in vitro in endothelial cells and murine aortic rings. Echocardiography and pressure / volume measurements revealed improved left ventricular ejection fraction, myocardial contractility, and diastolic function and decreased myocardial fibrosis after treatment. Concomitantly, numbers of capillaries and arterioles were increased. SWT resulted in enhanced expression of the chemoattractant stromal cell-derived factor 1 in ischemic myocardium and serum. Treatment induced recruitment of bone marrow-derived endothelial cells to the site of injury. In vitro, SWT resulted in endothelial cell proliferation, enhanced survival, and capillary sprouting. The effects were vascular endothelial growth factor receptor 2 and heparan sulfate proteoglycan dependent.
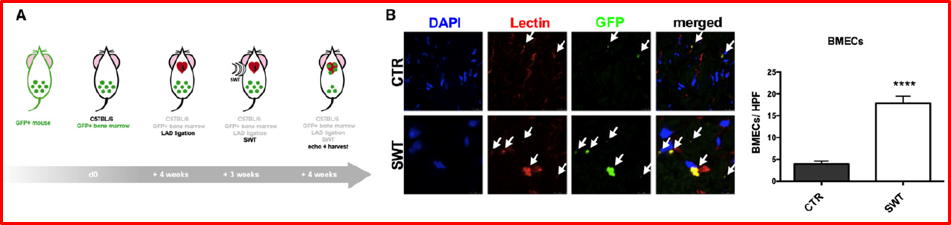
Figure 6. SWT stimulates cardiac vasculogenesis in chronic heart failure by recruitment of bonme marrow-derived endothelial cells. A, GFP bone marrow transplantation model for evaluation of myocardial angiogenesis. Wildtype animals underwent sublethal irradiation and receives a bone marrow transplantation of GFP (green fluorescent protein) donor mice. LAD ligation and after three weeks cardial SWT were performed. Four weeks later, hearts were harvested and analyzed for GFP-positive endothelial cells (representing bone-marrow derived endothelial cells. B, SWT recruitment and homing of bone marrow-derived endothelial cells (BMECs) to ischemic myocardium. Quantification of cells double-positive for rhodamine-labeled isolectin (red, endothelial cell marker) and for GFP (green, bone marrow-derived cells) revealed significantly higher numbers of BMECs in the treatment group compared with untreated controls.
Beneficial effects of Spark Wave Therapy:
- Spark Wave Therapy induces angiogenesis and arteriogenesis and upregulates pivotal angiogenic factors in vivo
- Spark Wave Therapy enhances cell survival and proliferation of endothelial cells
- Spark Wave Therapy improves ventricular ejection fraction
- Spark Wave Therapy improves myocardial contractility
- Spark Wave Therapy improves diastolic function
- Spark Wave Therapy decreases myocardial fibrosis
This high-quality, state of the art fundamental research study demonstrated that SWT could serve as a promoter of „endogenous cell therapy“ without exhibiting the disadvantages of cell harvesting necessary for conventional cell therapy. In addition, long-term effects of SWT are well known because it has been used in medicine for more than three decades. No severe side-effects were described after SWT. Thus, SWT for regeneration of ischemic myocardium could be translated into a clinical setting efficiently.
Reference:
Gollmann-Tepeköylü, C. et al. Shock wave therapy improves cardiac function in a model of chronic ischemic heart failure: Evidence for a mechanism involving vegf signaling and the extracellular matrix. J. Am. Heart Assoc. (2018). doi:10.1161/JAHA.118.010025