OBJECTIVE:
To determine the outcomes and mechanisms of delayed low-intensity extracorporeal shock wave therapy (Li-ESWT) in a rat model of irreversiible SUI. 1
MATERIAL AND METHODS:
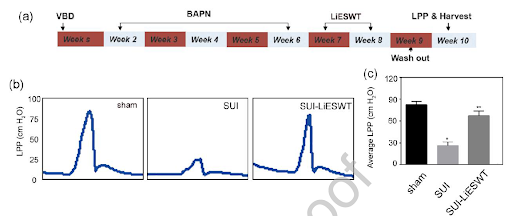
Twenty-four female Sprague-Dawley rats were randomly assigned into 3 groups: sham control, vaginal balloon dilation + β-aminopropionitrile (BAPN; SUI group), and vaginal balloon dilation + BAPN + treatment with Li-ESWT (SUI-Li-ESWT group). An irreversible SUI model was developed by inhibiting the urethral structural recovery with BAPN daily for 5 weeks. Thereafter, in the SUI-Li-ESWT group, Li-ESWT was administered twice per week for 2 weeks. After a 1-week washout, all 24 rats were evaluated with functional and histologic studies at 17 weeks of age. Endogenous progenitor cells were detected via the EdU-labeling method.
RESULTS:
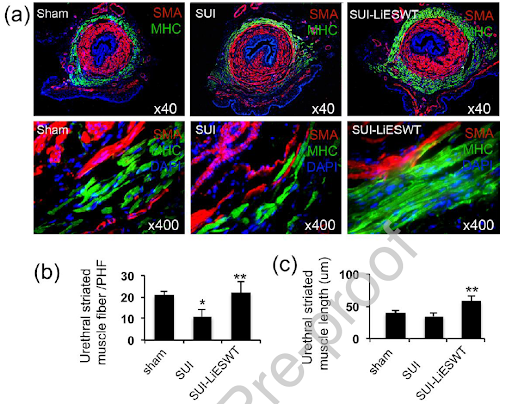
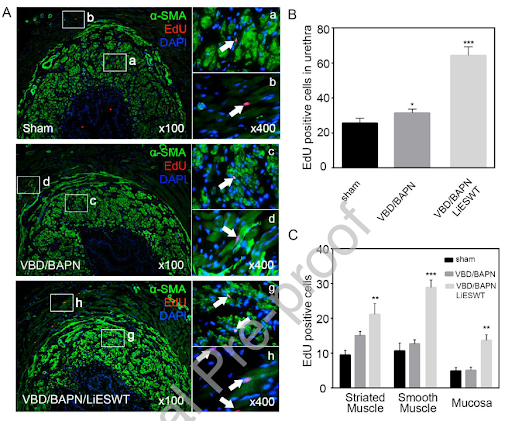
Functional analysis with leak point pressure testing showed that the SUI-Li-ESWT group had significantly higher leak point pressures compared with untreated rats. Increased urethral and vaginal smooth and striated muscle content and increased thickness of the vaginal wall were noted in the SUI-Li-ESWT group. The SUI group had significantly decreased neuronal nitric oxide /tyrosine hydroxylase positive nerves ratio in the smooth muscle layers of the urethra, while the SUI-Li-ESWT group had neuronal nitric oxide/tyrosine hydroxylase+ nerves ratio similar to that of the control group. The continuality of urothelial cell lining was also improved in the SUI-Li-ESWT group. In addition, there were significantly increased EdU-positive cells in the SUI-Li-ESWT group.
CONCLUSION:
Li-ESWT appears to increase smooth muscle content in the urethra and the vagina, increase the thickness of urethral wall, improve striated muscle content and neuromuscular junctions, restore the integrity of the urothelium, and increase the number of EdU-retaining progenitor cells in the urethral wall.
Beneficial effects of Spark Wave Therapy:
- Activation of stem / progenitor cells
- Regeneration of urethral and vaginal muscles
- Induced angiogenesis
- Restored functional and structural defects that contribute to SUI
- Non-invasive modality to facilitate tissue regeneration and improve voiding function
Reference:
- Zhang, X. et al. Delayed Treatment With Low-intensity Extracorporeal Shock Wave Therapy in an Irreversible Rat Model of Stress Urinary Incontinence. Urology (2020). doi:10.1016/j.urology.2020.03.035