1. Introduction
In modern society today, sport activity is becoming increasingly important. Reasons include more free time, increasing health awareness and a shifting biological age limit for sporty activities. Amateur sportsmen but especially high performance athletes are progressively affected by sport injuries.
 Sport orthopedics and traumatology
Sport orthopedics and traumatology
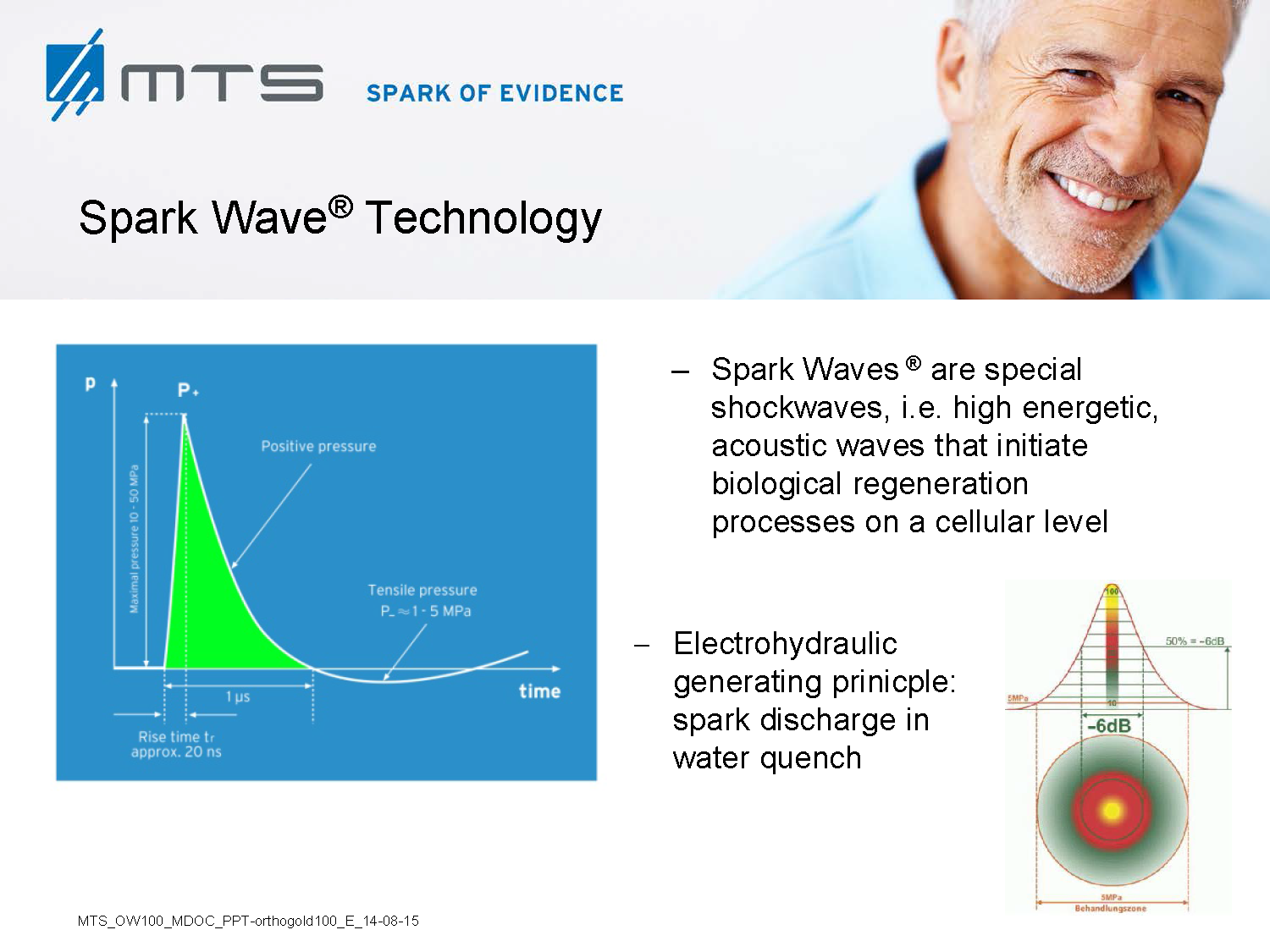
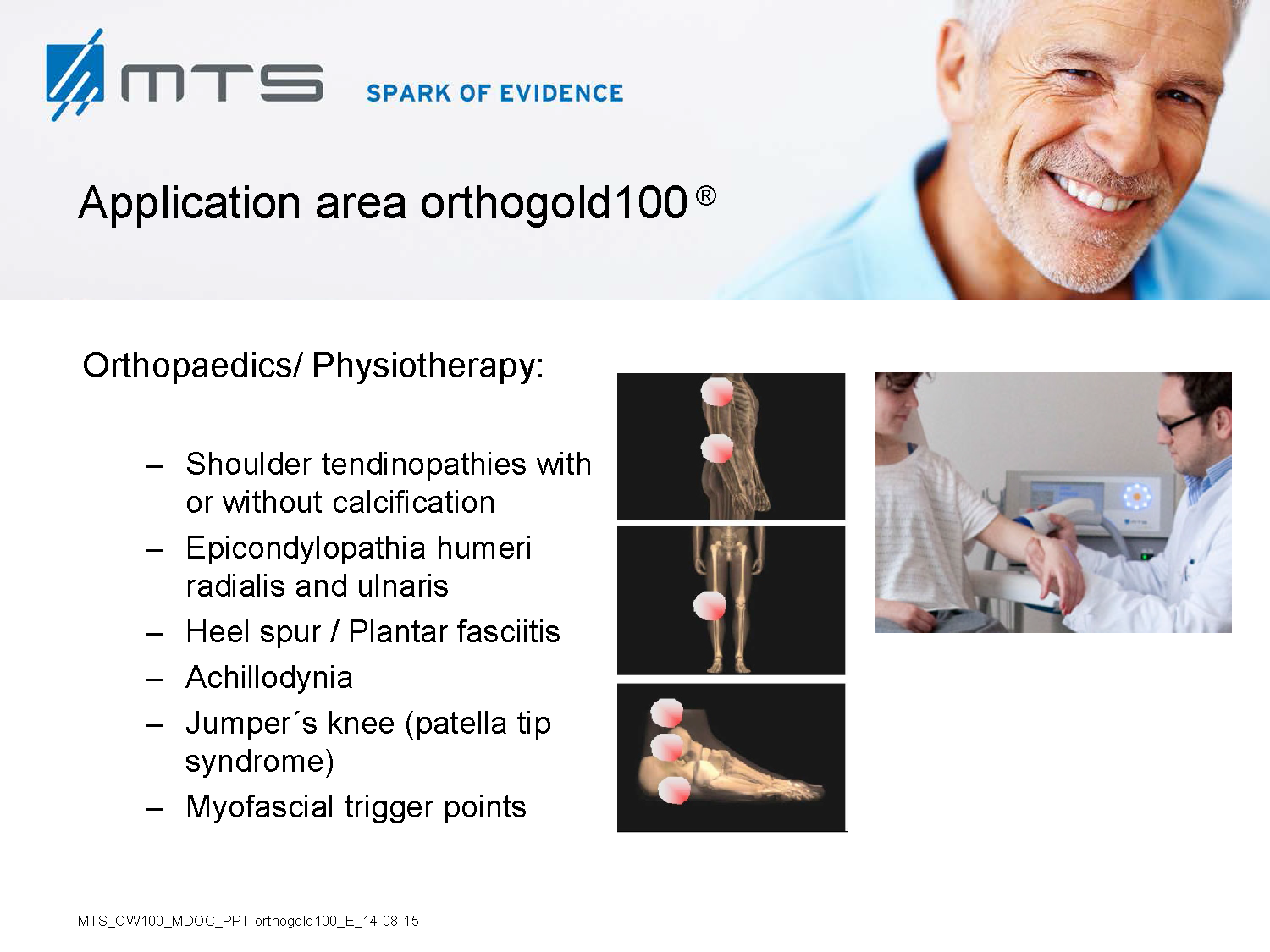
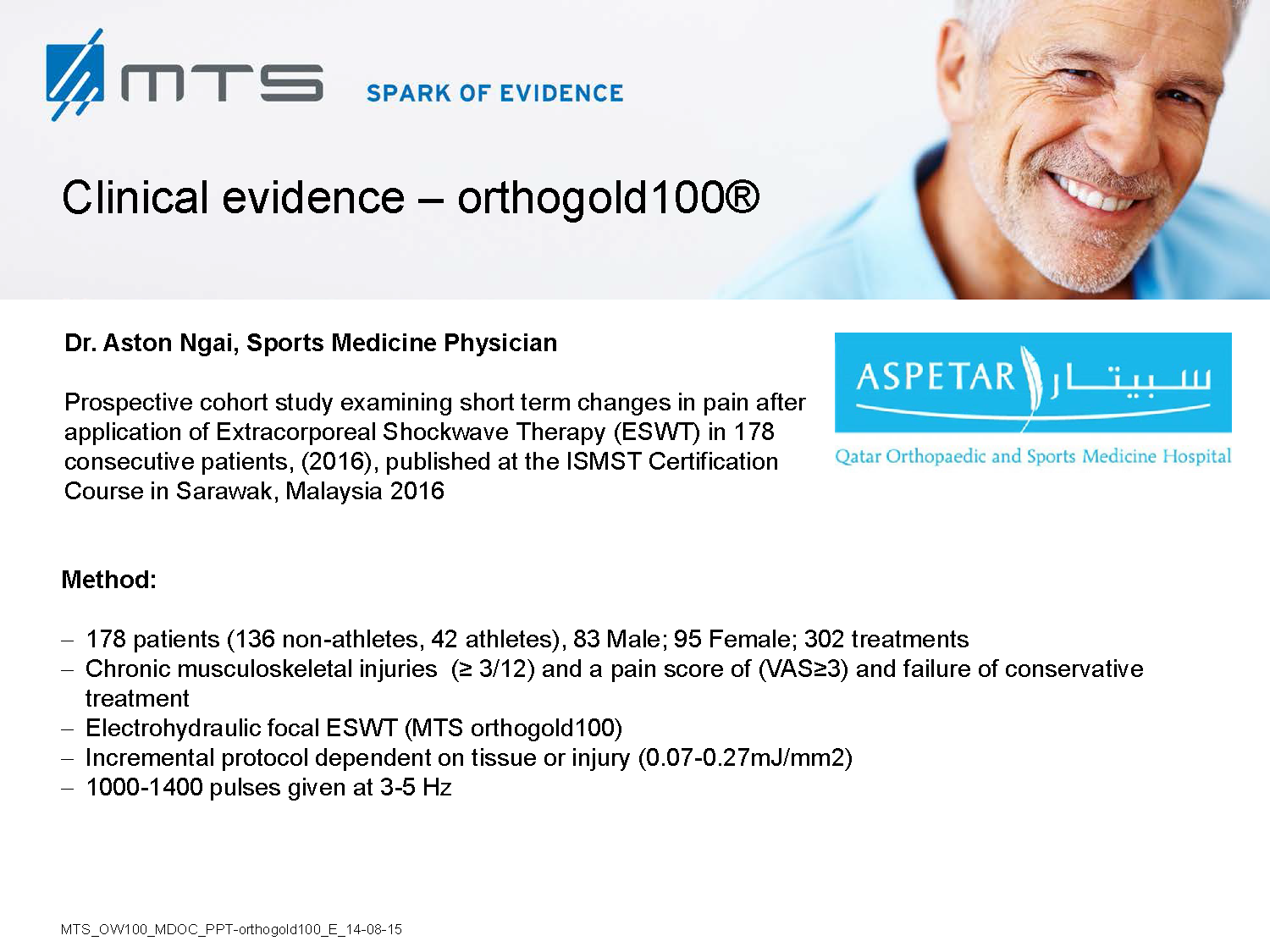
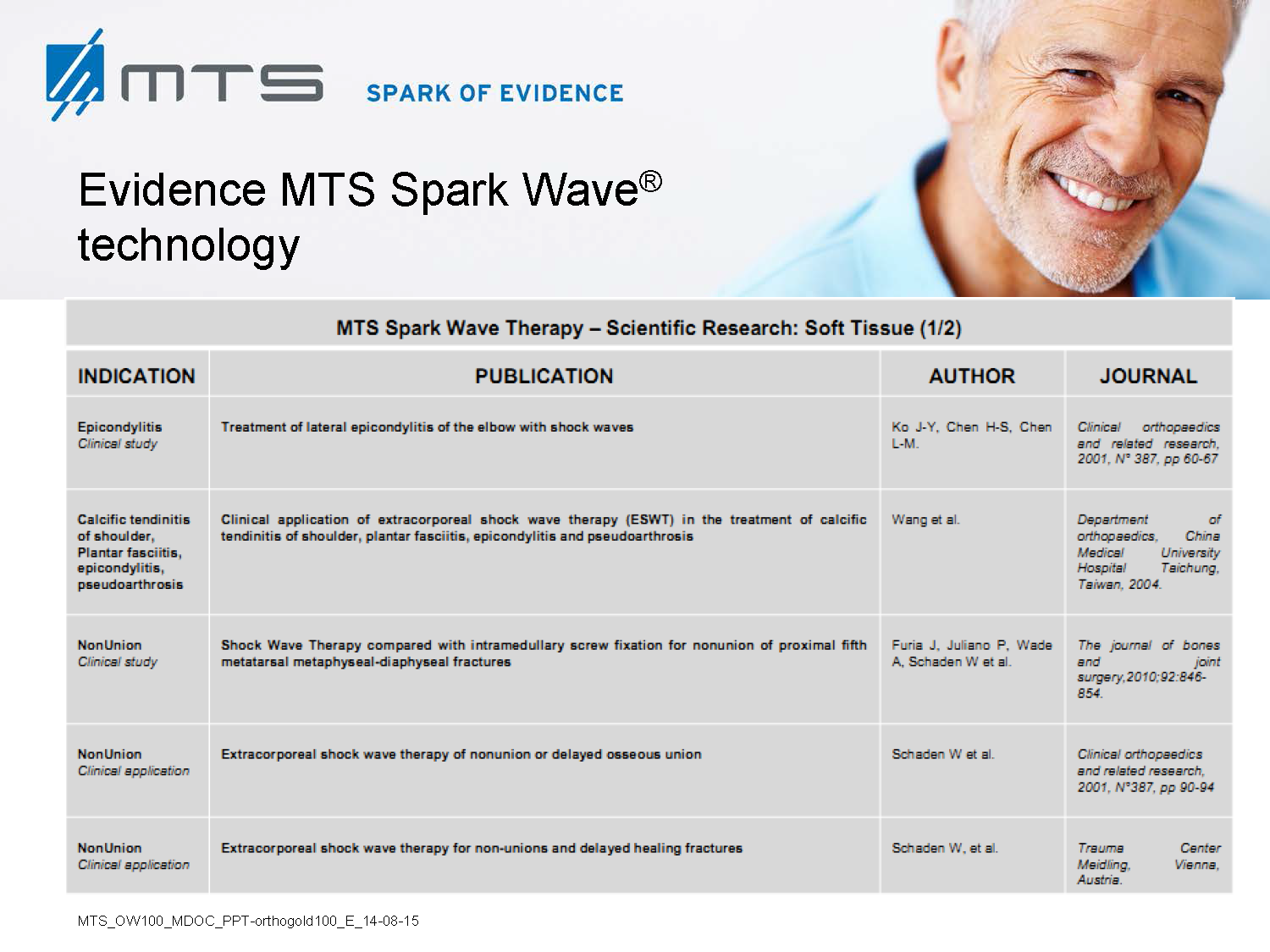
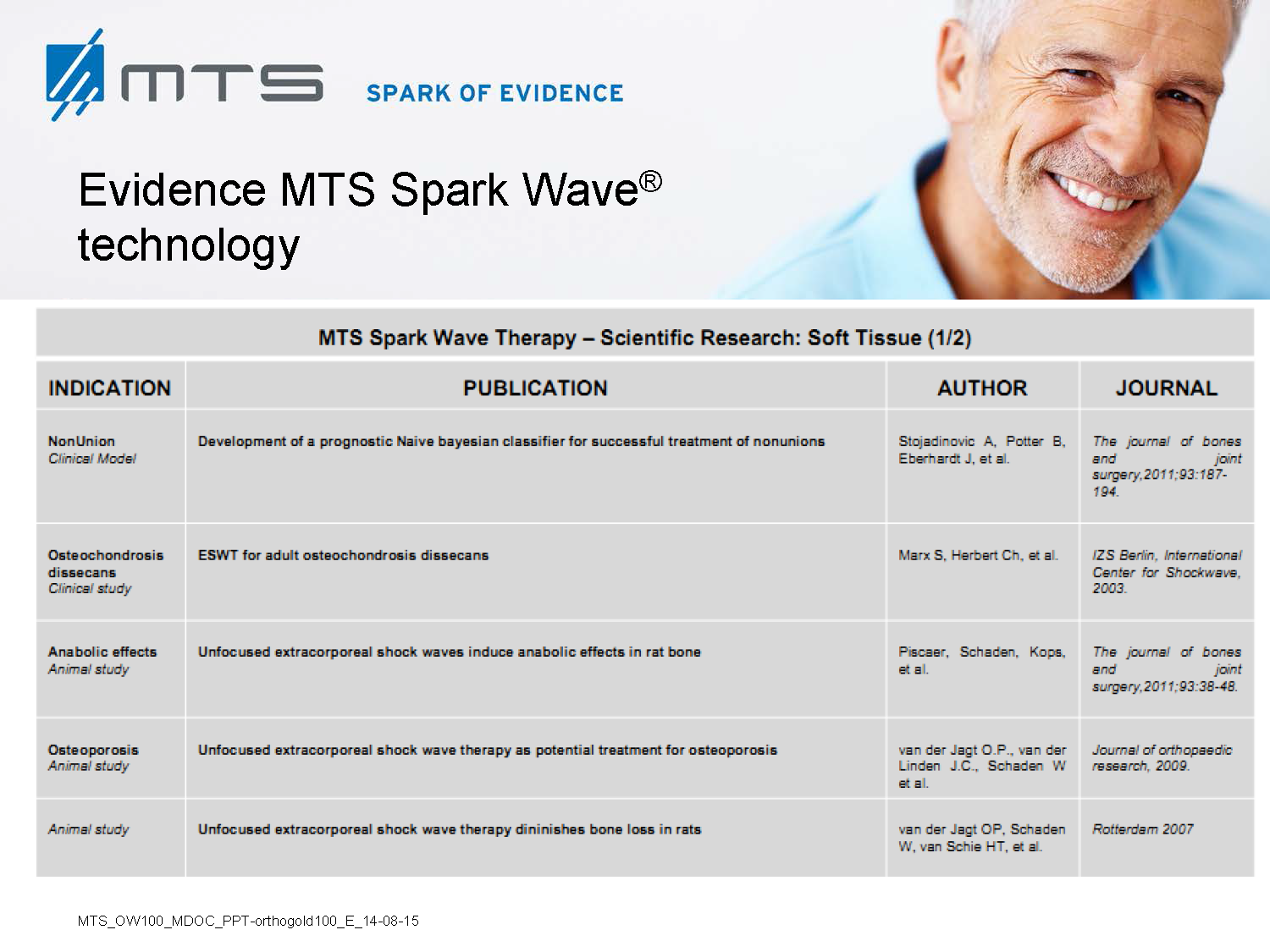
The extracorporeal generated shock wave therapy (ESWT) is the golden standard worldwide to treat urolithiasis. Nowadays, its curative effect is used for many other indications like musculoskeletal diseases, e.g. calcaneal spur, calcified shoulder, patella-tip syndrome, pseudoarthrosis and even bone fractures.
Furthermore, shock waves are widely used in wound healing to promote skin recovery of burns, diabetic foot ulcers and scars. The healing properties of shock waves originate from their wide-ranging tissue strengthening and regeneration effect, their acting analgesic and mobilizing, thereby increasing musculoskeletal capacity and performance.
Reasons for sports injuries are many and varied, dependent on the type of sport. Beside acute injuries (fractures, sprains etc.), particularly over-use problems (tendinopathies, degenerative diseases etc.) are becoming relevant during daily pratice of a sports physician. Is the actual burden exceeding the individual loading limit of the connective and supporting tissue of the athlete, it will lead to muscle- and tendon irritations, joint pains, inflammation and/or stress fractures. To avoid irreversible damages of soft tissues and joints, specific diagnosis and treatment is necessary. Particularly, professional athletes often suffer from long time existing chronic complaints.
2. Classic indications / pathologies in sports medicine
| Sport discipline | Musculoskeletal disorder | |
| Soccer, Baseball, Football, Rugby, Skiing |
Ø Bone fractures (collar bone, tibia & fibula, ellbow & wrist) Ø Pulled muscles and torn muscle fibers Ø Cartilage and articular capsule damage Ø Nerve damages Ø Torn & elongated ligaments (ankle / knee /shoulder joints & tendons, achilles tendon, heel pain etc…)
|
|
| Golfing | Ø Golfer tendinitis
Ø Epicondylitis humeri ulnaris („golfer elbow“) & Epicondylitis humeri radialis („tennis elbow“) & Hamulus ossis hamati („golfer wrist“) Ø Spine complaints & back pain, shoulder problems
|
|
| Handball | Ø Pulled muscles and torn muscle fibers
Ø Cartilage and articular capsule damage (rotator cuff, wrist…) Ø Torn & elongated ligaments (ankle / knee /shoulder joints & tendons, achilles tendon etc…)
|
|
| Running | Ø Patellar tendinopathies („runner`s or jumper`s knee“)
Ø Joint degeneration, knee arthritis Ø Pulled muscles and torn muscle fibers Ø Torn & elongated ligaments (ankle / knee / achilles tendon) Ø Stress fractures Ø Hip pain (avascular necrosis of the femoral head, trochanter pain syndrome) Ø Back pain, overload of the spine
|
|
| Biking | Ø Acute injuries of the skin and bruises
Ø Bone fractures (collar bone, tibia & fibula, ellbow & wrist) Ø Tensioning in the neck Ø Pain in the spine and muscles of the back Ø Numbness of limbs due to vibration and pressure load (nerve blockage) Ø Impingement syndrome, subacromial pain syndrome Ø Shoulder, rotator cuff, supraspinatus problems and instabilities |
|
| Tennis |
Ø „Tennis ellbow / arm“ (Epicondylitis humeri radialis) Ø Nervus ulnaris compression syndrome Ø Carpal tunnel syndrome (tendovaginitis), hand and wrist Ø Spinal pain and muscle injuries Ø Torn muscle fibers, cartilage & tendon injuries of the legs and knees
|
|
| Bodybuilding, weight lifting | Ø „Tennis ellbow / arm“ (Epicondylitis humeri radialis)
Ø Spinal pain and muscle injuries Ø Biceps tendinopathies |
|
3. Mechanotransduction mechanism of shock wave therapy
The original application of extracorporeal shock waves in medicine was the destruction of kidney stones by lithotripsy in 1980. During this procedure the tissue is exposed to high acoustic energy and much effort was spent to investigate its potential side effects. In consequence, destructive but also regenerative effects were observed 1. A dose-dependent effect was detected with high energy leading to more destructive effects and lower energy leading to more regenerative effects in the treated tissue 2,3. In the early 1990s, extracorporeal shock wave effects on bone and soft tissues led to indication of this treatment in musculoskeletal disorders 1. Since 2007, defocused shock waves were subjected to soft tissue indications with promising success 4,5.
Although the precise biomolecular mechanisms of shock waves in tissues are still under investigation, the underlying principle of its effect can be based on a mechanical stimulation that becomes transformed into a cellular regeneration and growth-associated response. In recent years, the field of “mechanobiology” emerged in the scientific field and researchers began to analyze the cellular effects of physical stimuli and to elucidate this mechanotransduction by which cells and tissues adapt their molecular behaviour due to mechanical signals 6. A quantity of mechano-sensitive molecules and cellular components that are involved in mechanotransductive biochemical responses have already been identified, such as stretchactivated ion channels, caveolae, integrins, cadherins, growth factor receptors, myosin motors, cytoskeletal filaments, nuclei, extracellular matrix, and numerous other structures and signaling molecules 7,8. It has been shown, that extracellular vesicles are released by mechanical shear stress and transfer miRNAs between cells 9,10. New evidence indicated that the mechanical stimulus of shock wave treatment causes exosome release of cells in vitro and is translated into a direct biological response leading to endothelial proliferation and angiogenesis (presented and published at the 4th ISMST basic research meeting in Vienna 2016 by Tepeköylü C et al., and the 20th international congress of the ISMST in San Sebastian 2017 by Graber M et al.) 9.
4. Biological response to shock wave application in regenerative sports medicine, research evidence
- Re-establishment of a functional vasculature is the most critical determinant of restored tissue structure and function in healing. It needs angiogenesis, endothelial sprouting and vasculogenesis. Shock waves stimulate the overall and muscular microcirculation 11–15. The treatment induces recruitment of endothelial progenitor cells and the expression of important angiogenic signalling factors like the vascular endothelial growth factor (VEGF) and nitric oxide (NO), a potent vasodilator 16– 23. The enhanced local blood flow protects against muscle soreness and pain, additionally stimulating muscle development and power 24.
- A main complaint of professional athletes is (chronic) local inflammation of tendons and joints. Shock waves lower the pro-inflammatory and induce the antiinflammatory profile in macrophages and alter the expression of cytokines and chemokines, like cyclophilin A, interleukins-6, -10 and -1β and of immune-receptors like the TLR3 (toll-like receptor 3) and other players 25–29. Furthermore, shock waves reduce leucocyte and macrophage infiltration and decrease the corresponding macrophagederived inflammatory protein response (MIP-1 α and β) 30,31. These experimental findings confirm that ESWT decreases the expression of high levels of inflammatory mediators 32.
- Apoptosis and necrosis. Avascular necrosis (osteonecrosis) in the hip or shoulder are bone defects caused by interruption of blood supply which leads to the death of cells in the bony matrix. In sports and athletic injuries, this is usually the result of trauma. The fact that SWT is able to enhance proliferation of MSCs and to induce their conversion into osteoblasts is an effective mechanism for treating avascular necrosis 33. Shock waves enhance the angiogenic and osteogenetic gene expression in bone marrow stromal cells from hips with osteonecrosis, an effect mediated by enhanced cell proliferation and increased VEGF, alkaline phosphatase, BMP2 (bone morphogenetic protein 2), RUNX2 (Runt-related transcription factor 2) and osteocalcin expression 34. Local SWT application results in significant elevations of serum NO level, angiogenic (VEGF, vWF, FGF and TGF-β1) and osteogenic (BMP-2, osteocalcin, alkaline phosphatase, DKK-1 and IGF) and anti-inflammatory (sICAM and sVCAM) factors in osteonecrosis 18,35,36. The process of bone repair along with restored blood supply in femoral or humeral head necrosis is accelerated by the use of extracorporeal shock waves.
- Regeneration, tissue remodelling and growth. Mesenchymal stem cells (MSC) represent one of the most promising tools in regenerative musculoskeletal tissue medicine 37. MSCs are responsible for the maintenance and regeneration of supporting and connective tissues, like bones, cartilage, muscles, ligaments, tendons and adipose tissue. Shockwaves activate recruitment, proliferation and differentiation of MCSs and thereby promote regeneration 33,38,39.
- Acute and fatigue fractures are frequent sport injuries. Shock waves enhance osteogenesis by activating growth and differentiation of bone marrow stromal cells towards osteoprogenitors with induction of TGF-ß1 (transforming growth factor), PCNA (proliferating cell nuclear antigen) and BMP-2 (bone morphogenetic protein) 40– 42. SWT has an anabolic effect in bones and leads to new bone formation via ERK and p38 kinase, playing a significant role in chondrogenesis and –protection and leading to enhanced bone mass and strength 41,43–47.
- Tendinitis and tendinosis are painful during moving and exercise. Shock waves stimulate tenocyte proliferation, collagen synthesis and extracellular matrix metabolism by early up-regulation of PCNA and TGF-beta1 gene expression and endogenous NO release 48. Tendon-derived stem progenitor cells proliferate and differentiate faster upon SWT, thereby increasing the efficiancy of tendon repair after injury 49,50. In tendinopathies shock waves trigger metabolic and regenerative events like rising glucosaminoglycan or lubricin levels and altering the inflammatory and catabolic profile of MMPs (matrix metalloproteinases) and Ils (interleukins) 51–53. SWT promotes removal of damaged matrix constitutents and enhances the resistance of tendons 53,54.
- The poor intrinsic regenerative capacity of articular cartilage makes it a great challenge to deal with cartilage defects and degeneration. SWT accelerates the healing rate and improves cartilage and subchondral bone quality 55. It facilitates the production of hyaline-like cartilage repair, via enhanced tenascin-C and chitinase 3like protein 1 (Chi3L1) expression and collagen synthesis 56,57. Shock waves delay progression of osteoarthtritis by reducing chondrocyte apoptosis and promote angiogenesis at cartilage end-plates without any structural damage to the joint 58–61.
- In musculoskeletal disorders, regeneration of injured muscles is very important. Demonstrated in murine and human myoblasts, shock waves induce muscle stem cell activation (proliferation, differentiation and migration) (Fuchs et al., 2017 ISMST San Sebastian). SWT leads to myogenesis and muscle regeneration, and enhances neovascularization at the tendon-bone junction 62–65. The improved circulation, the greater availability of oxygen and activation of the tissue directly also leads to an increased muscle performance 24.
Therefore, SWT can help to
- Regenerate injured muscles
- Relief muscle soreness and stiffness
- Prevent injuries and overuse syndromes by increasing muscle resilience
- Increase performance capacity and effectively improve the personal best
Furthermore, SWT represents a promising treatment approach to reduce age related muscle atrophy and enhance mobilty in older and hindered persons.
- Peripheral nerve injuries due to sports are relatively rare. Particular sports activities tend to cause certain peripheral nerve injuries including direct acute compression or stretching, repetitive compression and stretching over time, or another mechanism such as ischemia or laceration. These nerve lesions may be severe and delay or preclude the athlete’s return to sports, especially in cases with delayed diagnosis 66.
ESWT appears to have differential effects on peripheral nerves and has been proven to promote axonal regeneration 67. Both behavioral and immunohistochemical data show that shock wave treatment accelerates the recovery of muscle sensitivity and functionality and promotes regeneration of injured nerve fibers 68,69. SWT induces endogenous progenitor cell recruitment and Schwann cell activation which coincides with angiogenesis, tissue, and nerve generation in neurovascular injuries 70. Evidentially, shock waves do not threaten peripheral nerve integrity during treatment of muscles 71,72.
In the central nervous system, SWT promotes VEGF expression and improves locomotor recovery after spinal cord injury 73. It also increases the expression of neurotrophin-3 and neurotrophin-3 mRNA, and daily therapy facilitated the activity of macrophages and Schwann cells, which improves the survival and regeneration of neurons 74.
- Nociception and pain management. In most cases, diseases of the musculoskeletal system are accompanied by pain. Therefore, another primary goal of sports medicine and rehabilitation is fast pain relief and restoration of mobility to get the athlete back into play. SWT allows to reduce pain syndromes quickly and helps to prevent the recurrence of pain in the long-term period in patients 75. A potential mode of action is the neurotransmitter substance P, generally associated with intense, persistent and chronic pain. Since SWT reduces the levels of substance P, it may relay pain messages to the central nervous system and trigger pain relief 76. Decreased calcitonin gene-related peptide (CGRP) levels upon SWT provide another neuronal mechanism of reduced pain transmission 77.
Chronic myofascial pain syndrome (MPS) and trigger points are the main causes of pain in the back, neck, shoulder and limbs. Symptoms are due to hyperirritable nodules in musculoskeletal fibers that contract tightly and cut off their own blood supply, thereby impairing the sensory nerve endings (referred to as „metabolic crisis“) 78. Although the biomolecular basis of shock wave mechanisms are still not clear, the clinical evidence suggests that SWT could reduce the pain of MPS by pain signal alteration, promoting angiogenesis and increasing perfusion in ischemic tissues induced by sensitization of nociceptors and muscle ischemia 79.
The inclusion of Spark Wave Therapy into the individual treatment programs reduces the period of disability in sports and rehabilitation time of the patient.
5. Benefits of Spark Wave® Therapy in regenerative Sports Medicine & Athletics
- Non-invasive, pain-free treatment
- Highly suitable in combination with conventional therapies
- Effectivity comparable to conventional therapies
- In many cases as successful as surgery → non-invasive primary treatment alternative
- Circulation support, regenerative & anabolic action
- Anti-inflammatory effect
- Promotes wound healing
- Effective in the treatment of acute or chronic & treatment-resistant tendinopathies
- Preventive therapy with muscle strengthening effect
- Increasing performance capacitiy of the athlete
- Faster return to play
- Effective, user-friendly, patient-convenient and safe technology
- Satisfying long-term solution
6. List of references
- Lohrer, H., Nauck, T., Korakakis, V. & Malliaropoulos, N. Historical ESWT Paradigms Are Overcome: A Narrative Review. BioMed Research International 2016, (2016).
- Haupt, G. Use of Extracorporeal Shock Waves in the Treatment of Pseudarthrosis, Tendinopathy and Other Orthopedic Diseases. Urol. 158, 4–11 (1997).
- Rompe, J. D., Kirkpatrick, C. J., Küllmer, K., Schwitalle, M. & Krischek, O. Dose-related effects of shock waves on rabbit tendo Achillis: A sonographic and histological study. Bone Jt. Surg. 80, 546–552 (1998).
- Schaden, W. et al. Shock wave therapy for acute and chronic soft tissue wounds: a feasibility study. Surg. Res. 143, 1– 12 (2007).
- Dumfarth, J. et al. Prophylactic Low-Energy Shock Wave Therapy Improves Wound Healing After Vein Harvesting for Coronary Artery Bypass Graft Surgery: A Prospective, Randomized Trial. Thorac. Surg. 86, 1909–1913 (2008).
- d’Agostino, M. C., Craig, K., Tibalt, E. & Respizzi, S. Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. International Journal of Surgery 24, 147–153 (2015). 7. Ingber, D. E. Cellular mechanotransduction: putting all the pieces together again. FASEB J. 20, 811–827 (2006).
- Moosavi-Nejad, S. F., Hosseini, S. H. R., Satoh, M. & Takayama, K. Shock wave induced cytoskeletal and morphological deformations in a human renal carcinoma cell line. Cancer Sci. 97, 296–304 (2006).
- Davidson, S. M., Takov, K. & Yellon, D. M. Exosomes and Cardiovascular Protection. Drugs Ther. 31, 77–86 (2017).
- Hergenreider, E. et al. Atheroprotective communication between endothelial cells and smooth muscle cells through miRNAs. Cell Biol. 14, 249–256 (2012).
- Wang, C.-J., Wu, R.-W. & Yang, Y.-J. Treatment of diabetic foot ulcers: A comparative study of extracorporeal shockwave therapy and hyperbaric oxygen therapy. Diabetes Res. Clin. Pract. 92, 187–193 (2011).
- Mittermayr, R. et al. Extracorporeal Shock Wave Therapy (ESWT) Minimizes Ischemic Tissue Necrosis Irrespective of Application Time and Promotes Tissue Revascularization by Stimulating Angiogenesis. Surg. 253, 1024–1032 (2011).
- Kisch, T. et al. Remote effects of extracorporeal shock wave therapy on cutaneous microcirculation. Tissue Viability 24, 140–145 (2015).
- Kuo, Y. R., Wang, C. T., Wang, F. S., Chiang, Y. C. & Wang, C. J. Extracorporeal shock-wave therapy enhanced wound healing via increasing topical blood perfusion and tissue regeneration in a rat model of STZ-induced diabetes. Wound Repair Regen. 17, 522–530 (2009).
- Kisch, T. et al. Repetitive shock wave therapy improves muscular microcirculation. Surg. Res. 201, 440–445 (2016).
- Tepeköylü, C. et al. Recruitment of endothelial progenitor cells in chronic hind limb ischemia by extracorporeal shock wave therapy in rats. Surg. – Acta Chir. Austriaca 43, 13 (2011).
- Zhang, X., Yan, X., Wang, C., Tang, T. & Chai, Y. The dose-effect relationship in extracorporeal shock wave therapy: the optimal parameter for extracorporeal shock wave therapy. Surg. Res. 186, 484–92 (2014).
- Wang, C. J., Yang, Y. J. & Huang, C. C. The effects of shockwave on systemic concentrations of nitric oxide level, angiogenesis and osteogenesis factors in hip necrosis. Int. 31, 871–877 (2011).
- Mittermayr, R. et al. Extracorporeal shock wave therapy (ESWT) for wound healing: Technology, mechanisms, and clinical efficacy. Wound Repair and Regeneration 20, 456–465 (2012).
- Gotte, G. et al. Short-time non-enzymatic nitric oxide synthesis from L-arginine and hydrogen peroxide induced by shock waves treatment. FEBS Lett. 520, 153–155 (2002).
- Antonic, V., Mittermayr, R., Schaden, W. & Stojadinovic, A. Evidence Supporting Extracorporeal Shockwave Therapy for Acute and Chronic Soft Tissue Wounds. WOUNDS-A Compend. Clin. Res. Pract. 23, 204–215 (2011).
- Tepeköylü, C. et al. Shock wave treatment induces angiogenesis and mobilizes endogenous CD31/CD34-positive endothelial cells in a hindlimb ischemia model: Implications for angiogenesis and vasculogenesis. Thorac. Cardiovasc. Surg. (2013). doi:10.1016/j.jtcvs.2013.01.017
- Aicher, A. et al. Low-energy shock wave for enhancing recruitment of endothelial progenitor cells: A new modality to increase efficacy of cell therapy in chronic hind limb ischemia. Circulation 114, 2823–2830 (2006).
- Fleckenstein, J., Friton, M., Himmelreich, H. & Banzer, W. Effect of a Single Administration of Focused Extracorporeal Shock Wave in the Relief of Delayed-Onset Muscle Soreness: Results of a Partially Blinded Randomized Controlled Trial. Phys. Med. Rehabil. 98, 923–930 (2017).
- Sukubo, N. G., Tibalt, E., Respizzi, S., Locati, M. & d’Agostino, M. C. Effect of shock waves on macrophages: A possible role in tissue regeneration and remodeling. J. Surg. 24, 124–130 (2015).
- Holfeld, J. et al. Shockwave therapy differentially stimulates endothelial cells: implications on the control of inflammation via toll-Like receptor 3. Inflammation 37, 65–70 (2014).
- Cai, Z. et al. Effects of Shock Waves on Expression of IL-6, IL-8, MCP-1, and TNF-alpha Expression by Human Periodontal Ligament Fibroblasts: An In Vitro Study. Sci. Monit. 22, 914–921 (2016).
- Stojadinovic, A. et al. Angiogenic response to extracorporeal shock wave treatment in murine skin isografts. Angiogenesis 11, 369–380 (2008).
- Holfeld, J. et al. Low-energy shock wave treatment induces angiogenesis in ischemic muscle by stimulation of toll-like receptor 3 signaling. Hear. J. Acute Cardiovasc. Care 128, 61–62 (2013).
- Kuo, Y. R. et al. Extracorporeal shock wave treatment modulates skin fibroblast recruitment and leukocyte infiltration for enhancing extended skin-flap survival. Wound Repair Regen. 17, 80–87 (2009).
- Davis, T. A. et al. Extracorporeal shock wave therapy suppresses the early proinflammatory immune response to a severe cutaneous burn injury. Int Wound J 6, 11–21 (2009).
- Notarnicola, A. & Moretti, B. The biological effects of extracorporeal shock wave therapy (eswt) on tendon tissue. Ligaments Tendons J. 2, 33–37 (2012).
- Zhai, L. et al. Effects of Focused Extracorporeal Shock Waves on Bone Marrow Mesenchymal Stem Cells in Patients with Avascular Necrosis of the Femoral Head. Ultrasound Med. Biol. 42, 753–762 (2016).
- Yin, T.-C., Wang, C.-J., Yang, K. D., Wang, F.-S. & Sun, Y.-C. Shockwaves enhance the osteogenetic gene expression in marrow stromal cells from hips with osteonecrosis. Chang Gung Med. J. 34, 367–74 (2011).
- Ma, H. Z., Zeng, B. F., Li, X. L. & Chai, Y. M. Temporal and spatial expression of BMP-2 in sub-chondral bone of necrotic femoral heads in rabbits by use of extracorporeal shock waves. Acta Orthop. 79, 98–105 (2008).
- Ma, H. Z., Zeng, B. F. & Li, X. L. Upregulation of VEGF in subchondral bone of necrotic femoral heads in rabbits with use of extracorporeal shock waves. Tissue Int. 81, 124–131 (2007).
- Viganò, M. et al. Mesenchymal stem cells as therapeutic target of biophysical stimulation for the treatment of musculoskeletal disorders. Orthop. Surg. Res. 11, 163 (2016).
- Raabe, O. et al. Effect of extracorporeal shock wave on proliferation and differentiation of equine adipose tissue-derived mesenchymal stem cells in vitro. J. Stem Cells 2, 62–73 (2013).
- Chen, Y. J. et al. Recruitment of mesenchymal stem cells and expression of TGF-β1 and VEGF in the early stage of shock wave-promoted bone regeneration of segmental defect in rats. Orthop. Res. 22, 526–534 (2004).
- Wang, F. S., Yang, K. D., Chen, R. F., Wang, C. J. & Sheen-Chen, S. M. Extracorporeal shock wave promotes growth and differentiation of bone-marrow stromal cells towards osteoprogenitors associated with induction of TGF-beta1. Bone Joint Surg. Br. 84, 457–61 (2002).
- Cheng, J. H. & Wang, C. J. Biological mechanism of shockwave in bone. International Journal of Surgery 24, 143–146 (2015).
- Wang, F.-S. et al. Physical Shock Wave Mediates Membrane Hyperpolarization and Ras Activation for Osteogenesis in Human Bone Marrow Stromal Cells. Biophys. Res. Commun. 287, 648–655 (2001).
- Chen, Y. J. et al. Activation of extracellular signal-regulated kinase (ERK) and p38 kinase in shock wave-promoted bone formation of segmental defect in rats. Bone 34, 466–477 (2004).
- Van Der Jagt, O. P. et al. Unfocused extracorporeal shock waves induce anabolic effects in osteoporotic rats. Orthop. Res. 31, 768–775 (2013).
- Wang, C. J. et al. Extracorporeal shockwave therapy shows chondroprotective effects in osteoarthritic rat knee. Orthop. Trauma Surg. 131, 1153–1158 (2011).
- Wang, F. S. et al. Ras Induction of Superoxide Activates ERK-dependent Angiogenic Transcription Factor HIF-1α and VEGFA Expression in Shock Wave-stimulated Osteoblasts. Biol. Chem. 279, 10331–10337 (2004).
- Wang, C. J., Yang, K. D., Wang, F. S., Hsu, C. C. & Chen, H. H. Shock wave treatment shows dose-dependent enhancement of bone mass and bone strength after fracture of the femur. Bone 34, 225–230 (2004).
- Chao, Y. H. et al. Effects of Shock Waves on Tenocyte Proliferation and Extracellular Matrix Metabolism. Ultrasound Med. Biol. 34, 841–852 (2008).
- Vetrano, M. et al. Extracorporeal shock wave therapy promotes cell proliferation and collagen synthesis of primary cultured human tenocytes. Knee Surgery, Sport. Traumatol. Arthrosc. 19, 2159–2168 (2011).
- Leone, L. et al. Extracorporeal Shock Wave Treatment (ESWT) Improves In Vitro Functional Activities of Ruptured Human Tendon-Derived Tenocytes. PLoS One 7, (2012).
- BOSCH, G. et al. Effect of extracorporeal shock wave therapy on the biochemical composition and metabolic activity of tenocytes in normal tendinous structures in ponies. Equine Vet. J. 39, 226–231 (2007).
- Zhang, D., Kearney, C. J., Cheriyan, T., Schmid, T. M. & Spector, M. Extracorporeal shockwave-induced expression of lubricin in tendons and septa. Cell Tissue Res. 346, 255–262 (2011).
- Waugh, C. M. et al. In vivo biological response to extracorporeal shockwave therapy in human tendinopathy. Cell. Mater. 29, 268–80; discussion 280 (2015).
- Orhan, Z., Ozturan, K., Guven, a & Cam, K. The effect of extracorporeal shock waves on a rat model of injury to tendo Achillis. A histological and biomechanical study. Bone Joint Surg. Br. 86, 613–618 (2004).
- Lyon, R., Liu, X. C., Kubin, M. & Schwab, J. Does extracorporeal shock wave therapy enhance healing of osteochondritis dissecans of the rabbit knee?: A pilot study knee. Orthop. Relat. Res. 471, 1159–1165 (2013).
- Wang, Q. et al. Effect of low-energy shock waves in microfracture holes in the repair of articular cartilage defects in a rabbit model. Med. J. (Engl). 124, 1386–1394 (2011).
- Mayer-Wagner, S. et al. The effect of high-energy extracorporeal shock waves on hyaline cartilage of adult rats in vivo.
- Orthop. Res. 28, 1050–1056 (2010).
- Zhao, Z. et al. Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Orthop. Trauma Surg. 132, 1547–1553 (2012).
- Ertürk, C. et al. The effect of extracorporeal shockwaves on cartilage end-plates in rabbits: A preliminary MRI and histopathological study. Acta Orthop. Traumatol. Turc. 46, 449–454 (2012).
- Väterlein, N., Lüssenhop, S., Hahn, M., Delling, G. & Meiss, a L. The effect of extracorporeal shock waves on joint cartilage–an in vivo study in rabbits. Orthop. Trauma Surg. 120, 403–406 (2000).
- Byron, C. R., Benson, B. M., Stewart, A. A. & Stewart, M. C. Effects of radial shock waves on membrane permeability and viability of chondrocytes and structure of articular cartilage in equine cartilage explants. J. Vet. Res. 66, 1757–1763 (2005).
- Zissler, A. et al. Extracorporeal Shock Wave Therapy Accelerates Regeneration After Acute Skeletal Muscle Injury. J. Sports Med. 1–9 (2016). doi:10.1177/0363546516668622
- Wang, B. et al. Low-intensity extracorporeal shock wave therapy promotes myogenesis through PERK/ATF4 pathway. Neurourology and Urodynamics (2017). doi:10.1002/nau.23380
- Rinella, L. et al. Extracorporeal shock waves modulate myofibroblast differentiation of adipose-derived stem cells. Wound Repair Regen. 24, 275–286 (2016).
- Wang, C.-J., Huang, H.-Y. & Pai, C.-H. Shock wave-enhanced neovascularization at the tendon-bone junction: An experiment in dogs. Foot Ankle Surg. 41, 16–22 (2002).
- Tettenborn, B., Mehnert, S. & Reuter, I. Peripheral Nerve Injuries in Sports . Fortschritte der Neurol. Psychiatr. 84, 551– 567 (2016).
- Hausner, T. & Nógrádi, A. The use of shock waves in peripheral nerve regeneration: New Perspectives? Rev. Neurobiol. 109, 85–98 (2013).
- Mense, S. & Hoheisel, U. Shock wave treatment improves nerve regeneration in the rat. Muscle Nerve 47, 702–710 (2013).
- Hausner, T. et al. Improved rate of peripheral nerve regeneration induced by extracorporeal shock wave treatment in the rat. Neurol. 236, 363–370 (2012).
- Li, H. et al. Low-energy Shock Wave Therapy Ameliorates Erectile Dysfunction in a Pelvic Neurovascular Injuries Rat Model. Sex. Med. 13, 22–32 (2016).
- Manganotti, P., Amelio, E. & Guerra, C. Shock wave over hand muscles: a neurophysiological study on peripheral conduction nerves in normal subjects. Ligaments Tendons J. 2, 104–107 (2012).
- Rompe, J. D., Bohl, J., Riehle, H. M., Schwitalle, M. & Krischek, O. [Evaluating the risk of sciatic nerve damage in the rabbit by administration of low and intermediate energy extracorporeal shock waves]. Z Orthop Ihre Grenzgeb 136, 407–411 (1998).
- Yamaya, S. et al. Low-energy extracorporeal shock wave therapy promotes vascular endothelial growth factor expression and improves locomotor recovery after spinal cord injury. Neurosurg. 121, 1514–1525 (2014).
- Lee, J.-H. & Kim, S.-G. Effects of extracorporeal shock wave therapy on functional recovery and neurotrophin-3 expression in the spinal cord after crushed sciatic nerve injury in rats. Ultrasound Med. Biol. 41, 790–6 (2015).
- S. LITVINENKO, O. B. DOBROVOLSKY, V. V. KURSHEV, L.V. VESELOVA, G. V. D. EFFECTS OF EXTRACORPOREAL SHOCKWAVE THERAPY ON THE PAIN SYNDROME IN DISEASES AND INJURIES OF THE MUSCULOSKELETAL SYSTEM IN ATHLETES. Sport. Med. Res. Pract. doi:10.17238
- Maier, M., Averbeck, B., Milz, S., Refior, H. J. & Schmitz, C. Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Orthop. Relat. Res. 237–245 (2003). doi:10.1097/01.blo.0000030173.56585.8f
- Takahashi, N., Wada, Y., Ohtori, S., Saisu, T. & Moriya, H. Application of shock waves to rat skin decreases calcitonin gene-related peptide immunoreactivity in dorsal root ganglion neurons. Neurosci. Basic Clin. 107, 81–84 (2003).
- Ramon, S., Gleitz, M., Hernandez, L. & Romero, L. D. Update on the efficacy of extracorporeal shockwave treatment for myofascial pain syndrome and fibromyalgia. International Journal of Surgery 24, 201–206 (2015).
- Ji, H. M., Kim, H. J. & Han, S. J. Extracorporeal shock wave therapy in myofascial pain syndrome of upper trapezius. Rehabil. Med. 36, 675–680 (2012).